Decoding HEDIS® MY 2024 for success in MY 2025

Health plans are under increasing pressure to deliver measurable quality improvement while navigating regulatory shifts, operational complexity, and rising member expectations. While HEDIS® Measurement Year (MY) 2024 is now in the rearview mirror, the work of quality improvement never stops.
The focus now shifts to off-season projects and preparing for the next cycle. A thorough post-season review—analyzing what worked, identifying delays, and uncovering data gaps—can help plans develop targeted strategies to optimize future performance. By reflecting on challenges and achievements of MY 2024, staying ahead of key changes for the upcoming season, and continuously preparing for digital quality transformation, plans can set themselves up for success in MY 2025 and beyond. Here are a few strategies that can help.
Strengthening retrieval and closing gaps
Medical record retrieval remains a cornerstone of HEDIS success for hybrid measures. Several foundational strategies can improve efficiency and outcomes, including strengthening provider data, consolidating outreach efforts, and investing in digital connectivity. While digital retrieval is essential, flexibility remains key—meeting providers where they are, whether through digital or traditional methods, can significantly boost retrieval rates.
Equally important is building a feedback loop with providers. Sharing high-level results fosters transparency and encourages continued engagement. Within the plan, cross-departmental collaboration is also critical. By breaking down silos and sharing responsibility across teams, plans can streamline communication, improve data capture, and reduce the need for in-season chart retrieval.
When it comes to gap closure, start early. Engaging providers at the beginning of the measurement year allows more time to close gaps and improve outcomes. Plans should prioritize high-impact measures, leverage technology to reduce manual work, and offer flexible retrieval options, combining digital and traditional outreach methods, to minimize provider burden.
Navigating timeline and measure changes
Continuing the trend observed in recent years, several National Committee for Quality Assurance (NCQA) audit deadlines will move slightly earlier for MY 2025, though the final submission deadlines will occur two days later (Figure 1). Meanwhile, multiple measures are transitioning to electronic clinical data systems (ECDS) only reporting, including cervical cancer screening (CCS), childhood immunization status (CIS), and immunizations for adolescents (IMA), while the eye exam for patients with diabetes (EED) measure is shifting to administrative-only reporting.
New measures are also being introduced, such as blood pressure control for patients with hypertension (BPC-E), essentially transitioning the controlling high blood pressure measure into ECDS and expanding eligibility criteria, and two mammogram-related measures. These changes will require careful planning and data readiness to ensure accurate reporting and compliance.
|
Submission Task |
MY 2024 Deadline |
MY 2025 Deadline |
|---|---|---|
|
Stop all nonstandard supplemental data collection |
February 28, 2025 |
February 27, 2026 |
|
Auditor approval of all supplemental data |
March 28, 2025 |
March 27, 2026 |
|
Preliminary rates submitted in IDSS |
April 11, 2025 |
April 10, 2026 |
|
Audit review meetings completed |
April 25, 2025 |
April 24, 2026 |
|
Medical record abstraction finalized for MRRV |
May 2, 2025 |
May 1, 2026 |
|
Preliminary rate review responses completed |
May 9, 2025 |
May 8, 2026 |
|
MRRV review completed |
May 23, 2025 |
May 22, 2026 |
|
Plan-locked submissions in IDSS |
May 30, 2025 |
May 29, 2026 |
|
Medicare patient-level detail submitted to CMS |
June 13, 2025, 9:00 pm ET |
June 15, 2026, 9:00 pm ET |
|
Auditor-locked submissions in IDSS |
June 13, 2025, 9:00 pm ET |
June 15, 2026, 9:00 pm ET |
Figure 1. NCQA audit timelines for MY 2024 and MY 2025.
On-demand webinar: Decoding the HEDIS MY 2024 season
Embracing the digital future
The transition to digital quality measurement is well underway, with a target of full digital-only reporting by 2030. This shift breaks down into two key components: measure logic and data model. Traditional measures rely on vendor-coded logic and proprietary data models, while digital quality measures (dQMs) use standardized Clinical Quality Language (CQL) and the FHIR data model.
This shift promises greater standardization, interoperability, and efficiency, but it also requires preparation. Recent polling of Cotiviti clients revealed that the majority of plans either haven’t started or are just getting started on their FHIR data transformation, with cost, lack of internal knowledge, and lack of strategic alignment cited as key barriers. When asked at the recent Cotiviti Client Conference 2025 to describe the FHIR data available for quality reporting, nearly two-thirds respondents indicated they had not yet started integrating FHIR data at all.
Which of the below statements best describes the FHIR data you have available for quality reporting?
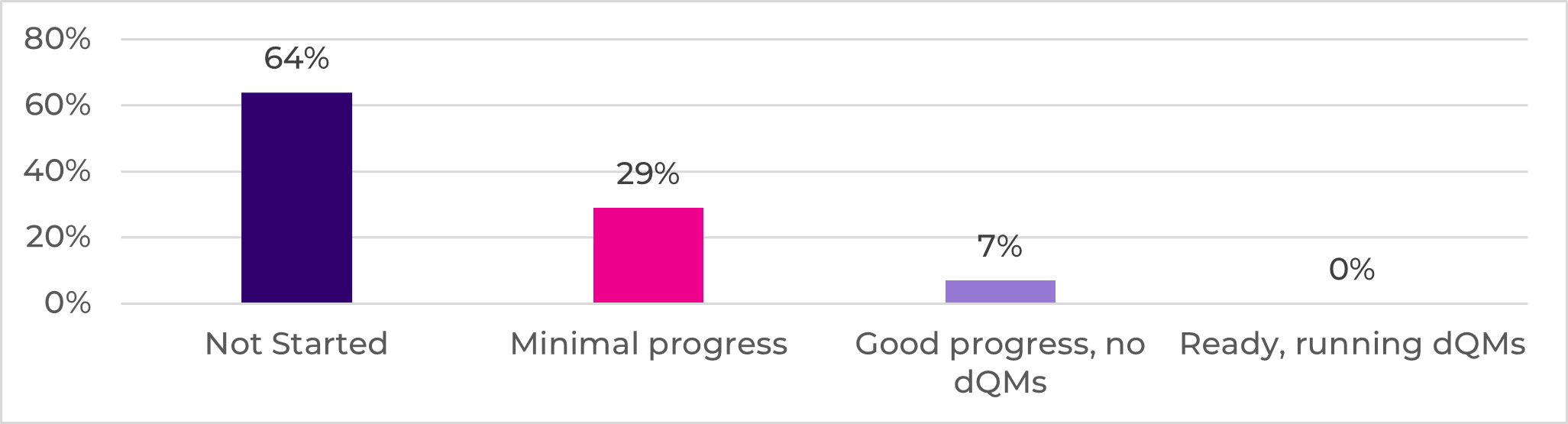
Figure 2. Cotiviti Client Conference 2025 poll of quality clients.
Health plans should take proactive steps now, such as identifying internal teams already working with FHIR, assessing data gaps, and building strategic alignment. Plans must work to help ensure they have the data they need to not only maintain the rates they produce today, but exceed them in the future.
An action plan for HEDIS success
Cotiviti is actively supporting clients through the transition to digital measurement with training, tools, workflows, and a roadmap for parallel reporting. As your organization works to meet the 2030 deadline, consider this phased approach:
- In the short term: Take inventory of FHIR readiness and evaluate downstream needs.
- Over the next 90 days: Attend a training on FHIR, build internal partnerships, and begin budgeting for necessary infrastructure.
- Over the next year: Monitor state-level digital reporting requirements, understand your data gaps, develop a plan for parallel reporting, and begin executing your strategy with continual refinement.
Reflecting on a year of milestones
Cotiviti’s Quality and Stars clients achieved significant HEDIS success in the recently concluded MY 2024 season. Every HEDIS client submitted ahead of the deadline, all retrieval projects exceeded their goals, and 100% of clients using Cotiviti for medical record abstraction passed the first round of medical record review validation (MRRV). These outcomes underscore the strength of Cotiviti’s partnerships and the value of early planning and collaboration.
With Cotiviti’s Quality Intelligence solution recently certified by NCQA for MY 2025, this year also marks Cotiviti’s 25th consecutive certification as a HEDIS vendor—a milestone that speaks to our long-standing commitment to quality and innovation.
To explore these strategies in more detail, watch our latest Quality Decoded webinar on demand as we dive deep into:
- MY 2024 successes
- MY 2025 challenges
- Critical HEDIS program updates to monitor
HEDIS® is a registered trademark of the National Committee for Quality Assurance (NCQA).
