Medical drug wastage and its impact on payment integrity
Jonathan Edwards | Jonathan Starr, PharmD | David Rullo, M.D.

Medical drugs are a vital component of healthcare delivery, but the dosage prescribed by a physician doesn’t always align with the amount in a single vial or package. The discarded quantity of a drug from a vial or package following administration to a patient is referred to as drug wastage—and it can be costly. Drug wastage is a key factor in rising healthcare costs, with some studies suggesting $3 billion in medications are wasted each year. For single-dose drugs, this remainder is unsalvageable for separate administration for several reasons, such as a lack of preservatives, issues with stability, or to ensure sterile administration. Neglecting to use the right vial or package can therefore mean that even the smallest amount of drug wastage adds up quickly over time.
The Center for Medicare & Medicaid Services (CMS) has been concerned about this matter for decades. In 2003, CMS developed the JW modifier to be appended to the drug codes that were billed to Medicare Administrative Contractors (MACs) so that wasted single-use drugs could be billed by providers, and CMS could get a refund from the drug manufacturer for this unused drug.
Drug wastage is a key factor in rising healthcare costs, with some studies suggesting $3 billion in medications are wasted each year.
Initially, reporting drug wastage with the JW modifier was only voluntary. But in 2017, following a lack of JW modifier use, CMS established a consistent policy on drug wastage and the use of the modifier, requiring that MACs enforce the policy with their providers. Following this requirement, on November 15, 2021, an amendment to the Infrastructure Investment and Jobs Act was passed that made it a requirement for manufacturers to refund CMS for the wasted drugs.
Despite these regulations, CMS still didn’t find drug wastage being reported as much as expected. Therefore, the agency developed the JZ modifier in 2023 to be reported in situations where the complete vial or package of the single-use drug was given to the patient, confirming a lack of wastage. By developing the JZ modifier and incorporating it into the CMS drug wastage policy, providers can clearly delineate the amount of drug provided to the patient and the amount of drug wastage.
Analyzing the increase in drug wastage modifier usage
Cotiviti analysis (Figure 1) shows that the utilization of the JW modifier has increased from 1.8% of medical drug claim lines in Q2 2023 (shortly after the JZ modifier was introduced) to 2.4% in Q3 2024. During the same period, use of the JZ modifier increased from 0.7% to 11.7%, driven by the CMS mandate effective July 2023.
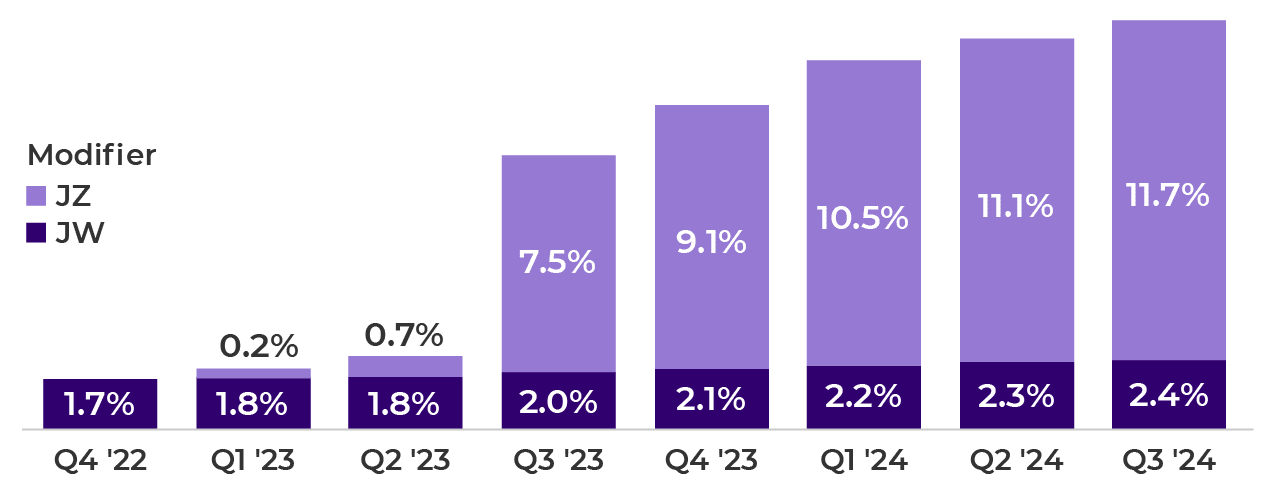
Our most recent data from Q3 2024 shows 14% of medical drug lines are billed with modifiers JW (2%) or JZ (12%). While it’s difficult to know what the optimal use of these modifiers should be since not all drugs are supplied in single-dose packages, there is evidence of room for improvement. According to Cotiviti’s data, approximately 30% of providers are using these modifiers to report drug wastage, with the top 5% of providers accounting for nearly 80% of the usage. Considering that the original intent behind the JZ modifier was to improve reporting of drug wastage, these low numbers appear to indicate that the majority of providers are still out of compliance. However, the silver lining is that provider adoption of JW has risen by 27% since the JZ modifier was mandated.
While only Medicare receives reimbursement from drug manufacturers based on reported drug wastage, all payers benefit from requiring the correct reporting of drug wastage to drive the most efficient use of expensive drugs.
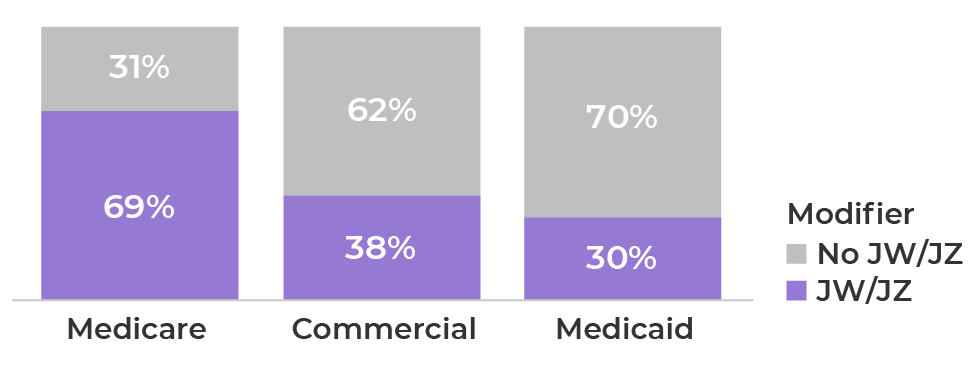
Since the JW and JZ modifier reporting requirements were mandated by CMS, it’s not surprising our data shows significantly more modifier use for Medicare than for commercial and Medicaid lines of business. Nearly 70% of Medicare medical drug spend is billed with drug wastage modifiers, compared to 38% and 30% for commercial and Medicaid, respectively (Figure 2).
(Oct 2023 – Sep 2024).
While only Medicare receives reimbursement from drug manufacturers based on reported drug wastage, all payers benefit from requiring the correct reporting of drug wastage to drive the most efficient use of expensive drugs. If no drug wastage policy were present, providers would have little motivation to limit the amount of waste that occurs. Multiple health plan representatives have confirmed to Cotiviti that they require reporting of drug wastage, regardless of line of business.
>50% of medical drug spend billed with JW/JZ modifiers linked to chemotherapies, shifting to other drug types
As expected, high-cost chemotherapy drugs account for more than half (52%) of the dollars spent with modifiers JW and JZ but make up only 18% of medical drug lines. Other agents include monoclonal antibodies, which drive another 20% of spend, followed by drugs for macular degeneration—both of which have increased in line count volume over the past two years (Figure 3).
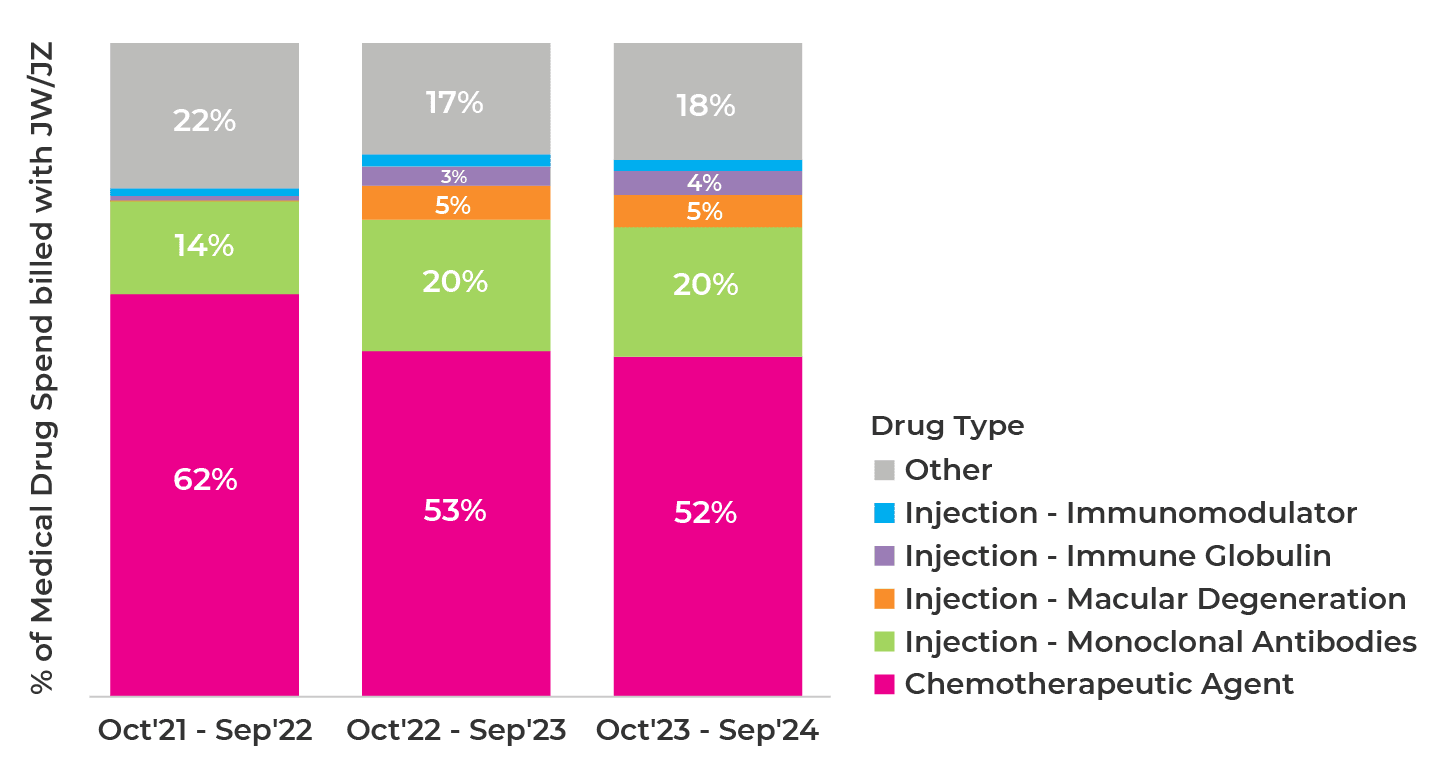
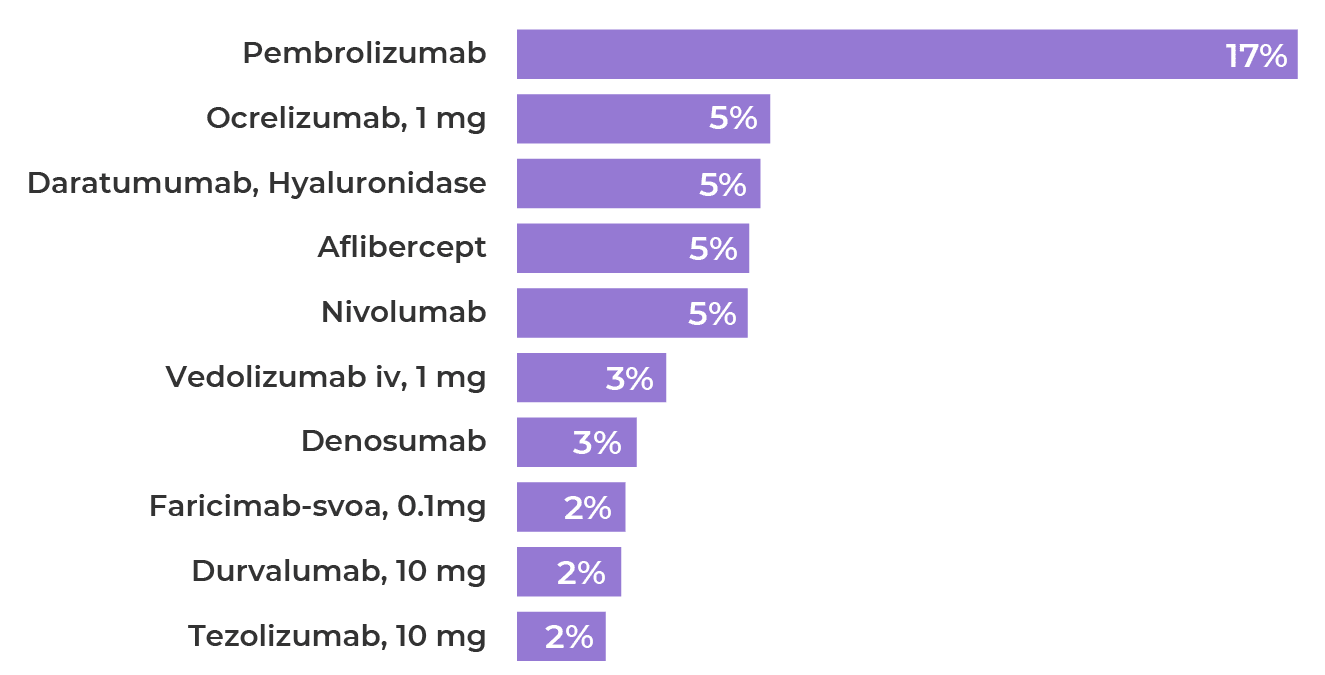
The top 10 medical drugs account for 49% of medical drug spend billed with JW or JZ (Figure 4), including pembrolizumab (J9271), a prominent chemotherapy drug used for multiple cancers. The remaining drugs treat multiple sclerosis (MS), gastrointestinal disorders, age-related macular degeneration (AMD), and a variety of cancers.
billed with JW/JZ modifiers.
Both healthcare professionals and outpatient facilities bill claims with drug wastage modifiers. Outpatient facility claims make up an average of about 65% of lines across Medicaid and commercial business, and almost half of Medicare lines (Figure 5).
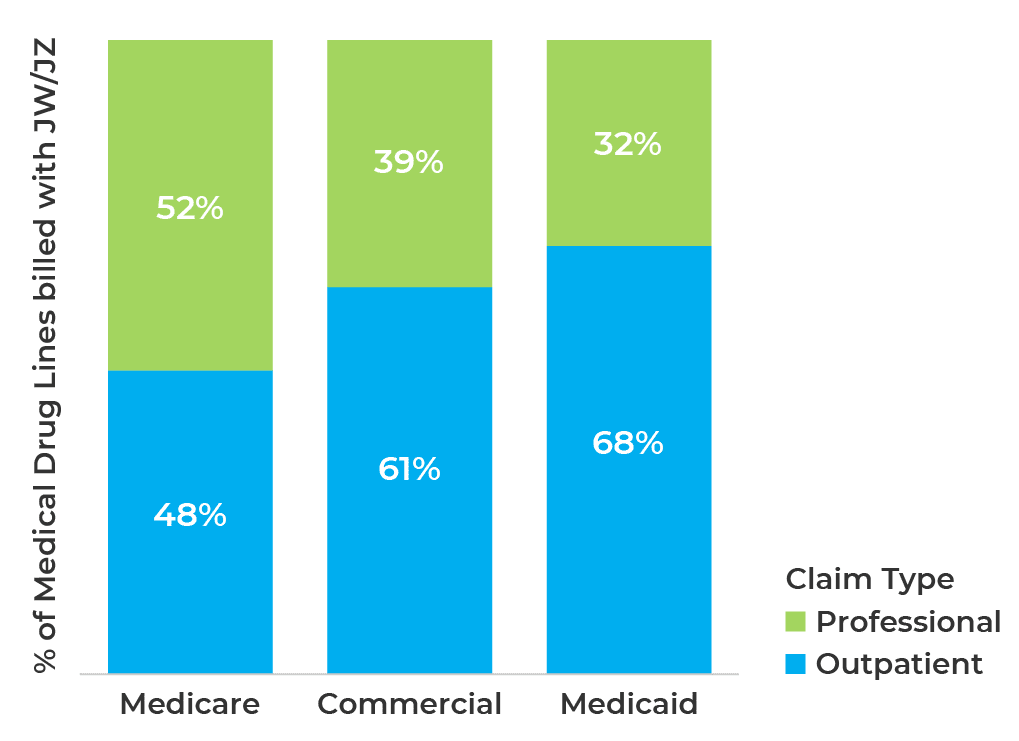
(Oct 2023 – Sep 2024).
Chemotherapy drugs account for 60% of outpatient medical drug spend billed with JW and JZ modifiers, including pembrolizumab, which alone contributes to 20%. For professional claims, hematology-oncology and ophthalmology specialties account for nearly 60% of spend billed with drug wastage modifiers. Notably, professional spend among ophthalmologists has increased from 2% to 20% in recent years, most likely due to complete use of drug packages for macular degeneration, including aflibercept (J0178) and faricimab (J2777). These two drugs comprise over 80% of the professional ophthalmologic spend billed with the JZ modifier.
Drug-specific payment policies capture >50% of payment integrity savings on lines billed with JW, JZ
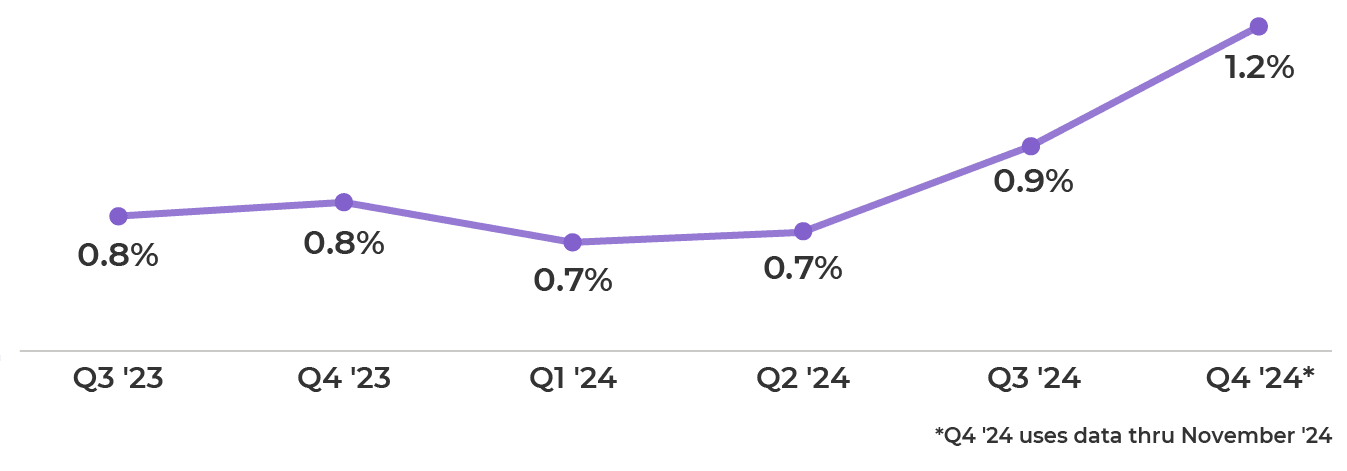
Cotiviti has developed a robust policy set in our Payment Policy Management prepay solution to enforce proper coding of drugs that require reporting of drug wastage. Drug-specific payment policies account for 50% of savings on lines billed with JW or JZ modifiers, including targeted policies that identify JW and JZ modifier coding errors for multi-dose and single-dose packages (vials). Our clients have increased their use of these drug wastage policies since 2023, reflected by a 71% increase in medical cost savings (from 0.7% to 1.2%) on lines billed with JW or JZ modifiers (Figure 6). With enhanced policy sets to enforce the proper reporting of drug wastage, we expect this trend to continue.
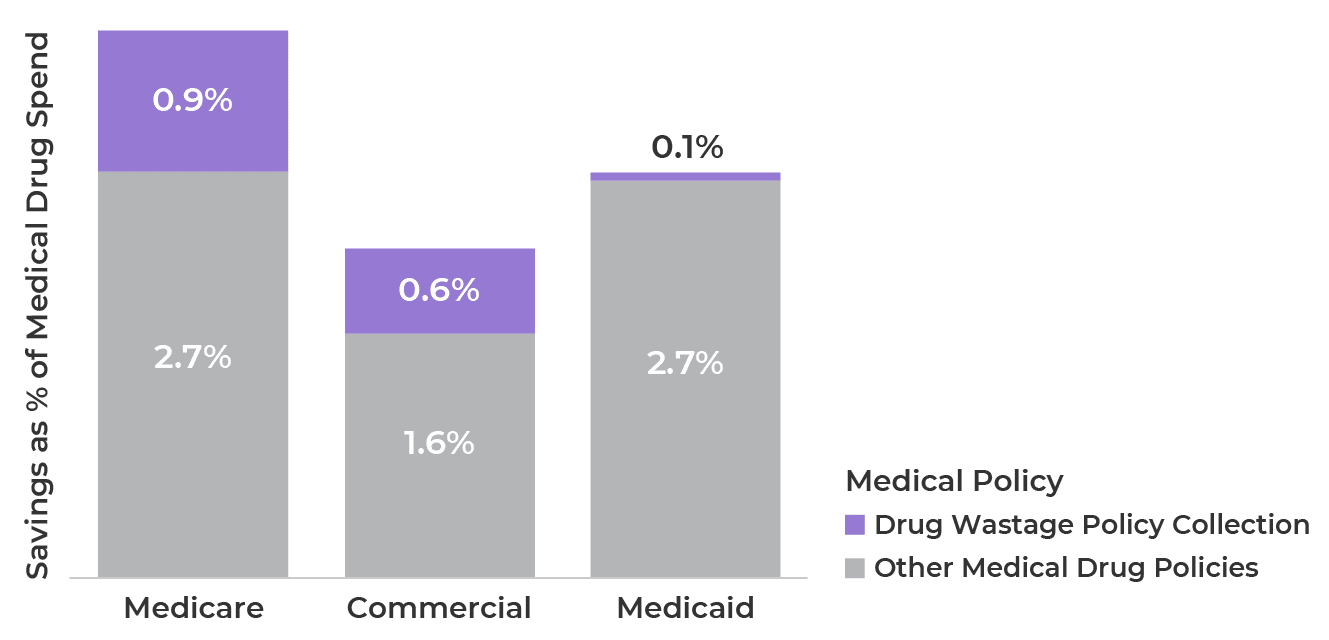
Comprehensive drug wastage payment policies can capture >30% more payment integrity savings
As our clients adopt more drug wastage policies, we have found that their total prepay payment integrity savings on medical drugs increases significantly. Our top clients in terms of drug wastage policy use have generated upwards of 30% more savings on medical drugs, depending on the line of business (Figure 7).
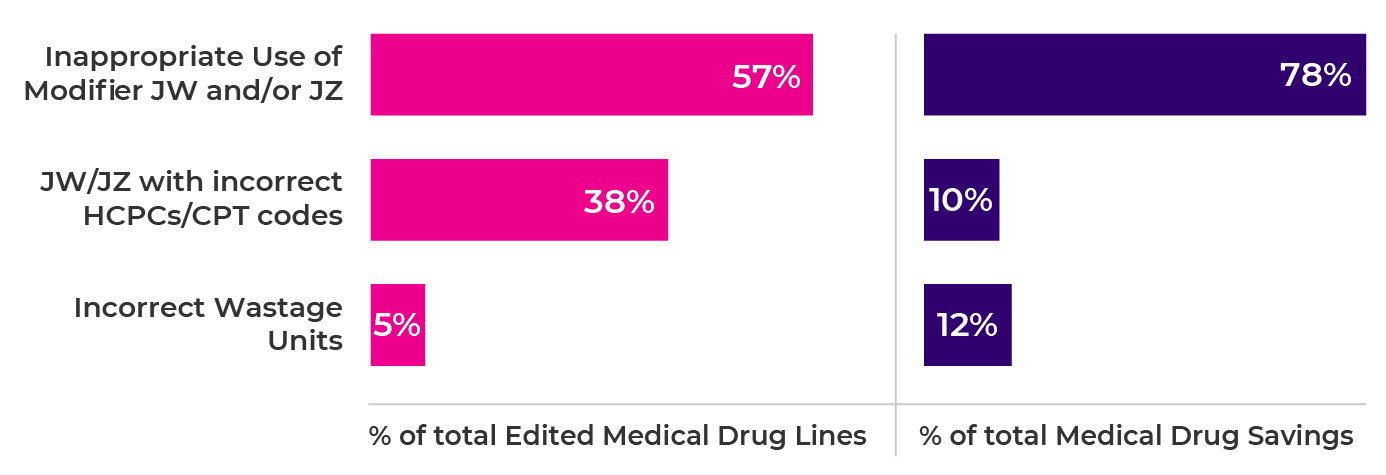
Cotiviti's drug wastage policies enforce correct coding in three ways:
- Inappropriate or lack of use of JW and JZ modifiers
- Use of JW and JZ modifiers with incorrect HCPCS/CPT codes
- Incorrect or excessive wastage units billed
As our clients adopt more drug wastage policies, we have found that their total prepay payment integrity savings on medical drugs increases significantly.
Our data shows most billing errors occur due to inappropriate use of the modifiers, contributing 57% of all edits and 78% of savings from such policies (Figure 8).
Improve modifier use and optimize payment integrity
Drug wastage claim modifiers are designed to help plans manage medical drug spend. As medical drug spend (>10% of total medical spend) continues to grow faster than other medical spend categories, using these modifiers appropriately is critical. While the use of JW and JZ modifiers is increasing, it is still isolated, and room exists for improvement.
Drug wastage modifiers are most commonly reported on claims for chemotherapies, however use is expanding to treatments for macular degeneration (AMD), multiple sclerosis (MS), and other complex conditions. As these categories continue to grow, payment policies that target inappropriate use of JW and JZ modifiers can help payers capture upwards of 30% more payment integrity savings on medical drugs. Make sure your plan is ready for the future, and ensure you have payment policies for JW and JZ modifiers built into your payment integrity program.
Specialty drugs and biologicals account for more than half of all prescription drug spending, and drug wastage is a key factor in rising healthcare costs. If you’re interested in your plan’s drug wastage trends, reach out to your Cotiviti client partner for a discussion.
If you’d like to know more about Cotiviti’s policies for improper specialty drug and biologic claims overall, read our overview of the Drug & Biological Policy Collections.
About the authors
|
|
Jonathan Edwards Jon leads a talented team of analytic professionals that deliver actionable insights powering Cotiviti’s most important growth opportunities. With more than 15 years of healthcare analytics and consulting experience, Jon harnesses the power of data to develop leading-class analytic products and services that inform decision-making, accelerate growth, and differentiate Cotiviti’s value proposition. |
 |
Jonathan Starr, PharmD Jonathan directs a team of pharmacy specialists in developing new content related to pharmacy claims. He also supports Cotiviti’s vast library of Drugs and Biological payment policies and aids in presenting these policies to clients. |
 |
David Rullo, M.D. Dr. Rullo is responsible for helping clients to understand payment policies while gleaning insights and value from their analytics. He has more than 30 years of experience in the healthcare industry, creating, maintaining and supporting software systems that analyze and correct physician and facility coding and practice patterns, including work at ProfSoft and McKesson. Dr. Rullo earned his medical degree at Boston University and was in surgical residency at the University of Massachusetts Medical Center in Worcester, Massachusetts. |