The shift to outpatient care
Jonathan Edwards | John Smith, M.D.

As healthcare continues to transform, the industry has observed a steady and significant shift from inpatient to outpatient care settings. This trend, driven by the Centers for Medicare & Medicaid Services (CMS) removal of procedures from the Inpatient Only List, advances in technologies, an increase in telehealth monitoring, value-based provider contracts, and patient preferences—is reshaping the landscape of medical care delivery.
As procedures that were once strictly performed in hospitals are now moving to outpatient facilities, patients and providers alike are witnessing a shift that promises both opportunity and challenges. Dive into the key drivers behind this change as we explore data trends and examine the implications for patient care and healthcare costs.
Outpatient spend continues to grow across all lines of business
Since 2022, outpatient care has seen a notable increase in spending share and utilization. This trend is driven in part because outpatient settings, including ambulatory surgery centers (ASCs), offer more convenient and cost-effective care than acute-care Inpatient hospitals.
As outpatient care continues to rebound from the COVID-19 pandemic and more procedures move to the outpatient setting, outpatient spend continues to grow and now accounts for up to 46% of ambulatory medical spend (Figure 1).
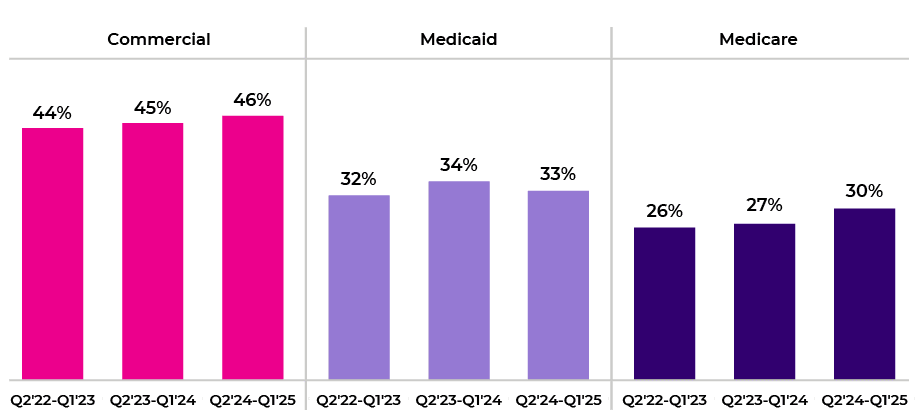
Figure 1. Contribution of outpatient medical spend to total ambulatory medical spend.
According to a recent report from KFF, inpatient admissions have dropped by almost 17% since 2000, with outpatient visits facing a steady increase of 23% from 2020-2023. Cotiviti’s client claim data shows this upward trend has continued over the last 3 years, with outpatient utilization rising to 4% annually, led by commercial plans (Figure 2).
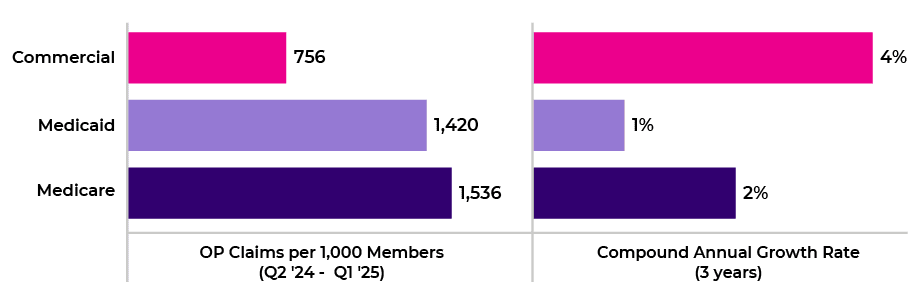
Figure 2. Change in outpatient utilization across line of business.
Increase in outpatient utilization is driven by musculoskeletal procedures and medical drugs
The shift to outpatient facilities can be attributed to factors such as advancements in minimally invasive surgical techniques and the economic incentives of a value-based care model. Innovations in medical technology and drugs have been pivotal in enabling procedures that once required inpatient care to be performed in outpatient settings.
Technological advances and incentives have notably increased musculoskeletal procedures in outpatient facilities, leading to lower surgical procedure costs. The scope of outpatient surgical options has expanded with minimally invasive laparoscopic techniques, improved anesthesia methods, and hybrid operating rooms.
According to a report from Sg2 Analytics, demand for adult outpatient care is expected to rise 17% by 2034, led by behavioral health, cardiovascular, neurology, and surgical procedures. This coincides with Cotiviti data that shows high compound annual growth rates (CAGR) of 10% and 14% for musculoskeletal and cardiovascular claims, respectively (Figure 3).
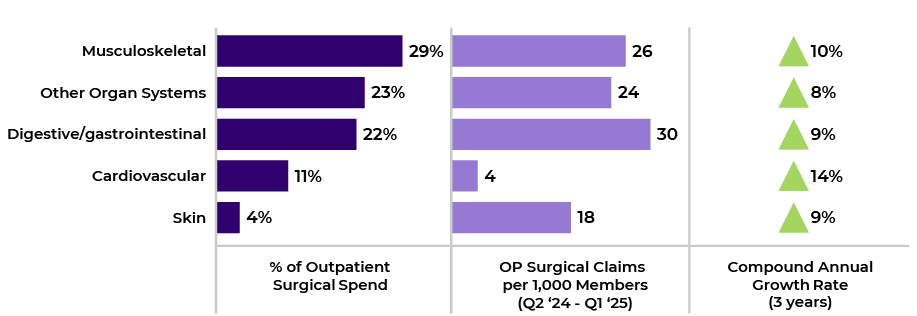
Figure 3. Trend in utilization for top five outpatient surgical code groups.
Advancements in chemotherapy drugs have contributed to a 9% increase in outpatient medical drug utilization. Keytruda (Pembrolizumab) alone contributes to 15% of outpatient medical drug spend, and use of this drug has increased 10% annually (Figure 4 ). This trend highlights the role of advanced pharmaceuticals in driving outpatient care adoption.
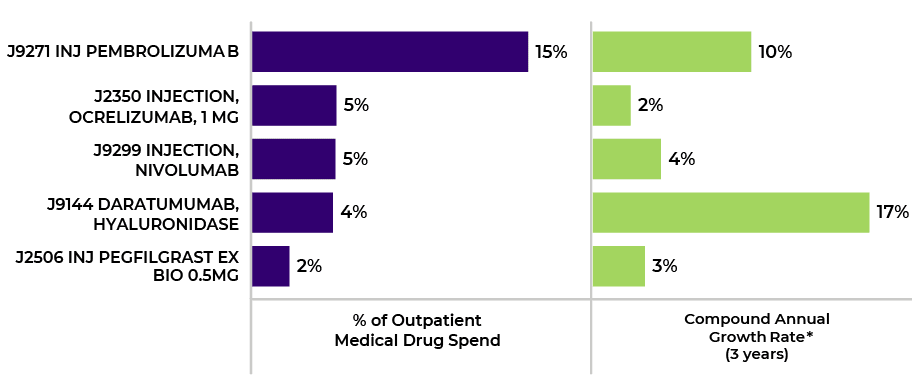
Figure 4. Key medical drugs driving increase in outpatient spend and utilization.
Cotiviti clients successfully mitigate the impact of increased outpatient spend
The shift to outpatient care brings numerous benefits, including cost savings, improved patient satisfaction, and more efficient use of healthcare resources. Additionally, the overall cost of care is reduced, benefiting both patients and insurers. But investing in training and infrastructure to handle the growing volume of outpatient procedures can prove costly and time consuming for payers, putting strain on already limited internal resources.
Payers that implement comprehensive outpatient payment integrity programs including prepay modifier review, surgical payment policies, and medical drug edits can successfully reduce outpatient spend, correct billing errors due to improper coding, and mitigate the impact of increased costs. For instance, health plans with prepay outpatient modifier review generate savings of up to 0.3% of outpatient spend, depending on line of business, with most billing errors related to incorrect coding. Since 2022, outpatient savings have increased 3% overall, with Medicare showing the highest increase in savings, followed by Medicaid (Figure 5). Savings rates are generally higher for Medicare and Medicaid due to negotiated rates with providers, lower cost share, site of care differences, and supplemental payments.
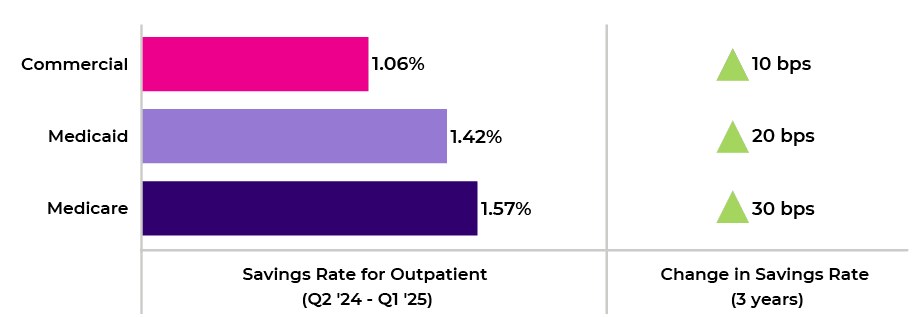
Figure 5. Change in outpatient savings rate across line of business.
Cotiviti data shows a broad range of claim editing performance on outpatient claims, with an inter-quartile range (25th to 75th percentile) of 0.6% to 1.8% medical cost savings, including many payers above 2% . In a comparison of the top and bottom quartile by editing performance, Cotiviti data revealed that the top quartile has higher edit rates on medical policies, adopts approximately twice as many decision points (DPs), and displays lower adjustment rates by applying a more comprehensive policy (Figure 6).
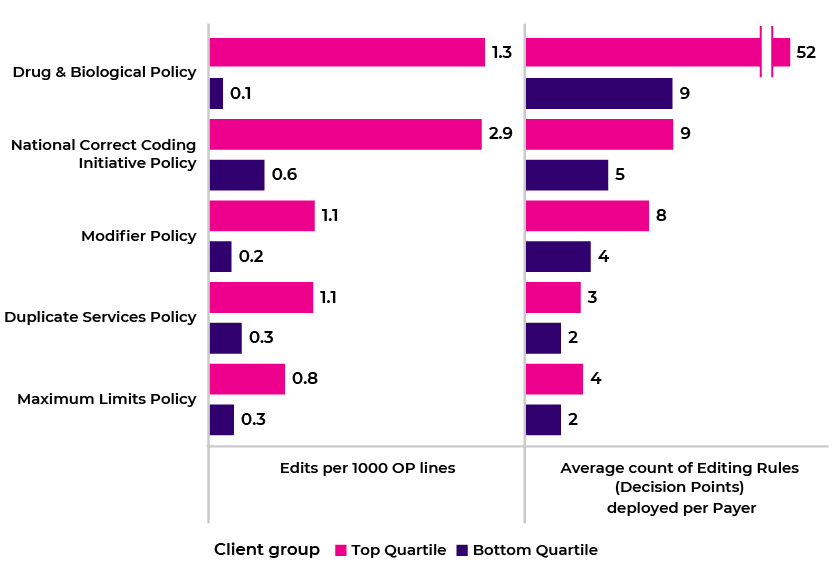
Figure 6. Difference in policy performance and adoption between top and bottom quartile payers.
The ongoing shift from inpatient to outpatient care is transforming the healthcare landscape, offering opportunities to improve patient outcomes and reduce costs. As outpatient care continues to evolve, healthcare organizations must address the challenges of accessibility, safety, and infrastructure. By adopting innovative policies and leveraging data-driven insights, providers and payers can ensure that this transition benefits all stakeholders.
Reduce inappropriate modifier use and improve your payment integrity with Cotiviti's Coding Validation solution for quick prepay outpatient facility claim review. Read our Payment Policy Insights article to discover how Coding Validation creates additional medical cost savings from identifying complex coding errors.
Cotiviti’s Clinical Chart Validation solution delivers a comprehensive program of complex prospective and retrospective claim reviews of inpatient DRGs. Read the blog to learn more about postpay reviews of outpatient claims, inpatient rehabilitation, and readmission claims.
About the authors
|
|
Jonathan Edwards Jon leads a talented team of analytic professionals that deliver actionable insights powering Cotiviti’s most important growth opportunities. With more than 15 years of healthcare analytics and consulting experience, Jon harnesses the power of data to develop leading-class analytic products and services that inform decision-making, accelerate growth, and differentiate Cotiviti’s value proposition. |
 |
John Smith, M.D., FAAFP, CPC, CHIE Dr. Smith leverages his extensive experience in both clinical practice and healthcare management in his role with Cotiviti. A family physician by training, he earned his medical degree from the Brody School of Medicine and completed his residency at Pitt County Memorial Hospital in Greenville, North Carolina. With nearly 20 years of clinical experience across various settings and an equal number of years in health plan roles, he has developed a comprehensive understanding of healthcare delivery systems. His current focus is on collaborating with clients to understand their data, priorities, and challenges, while analyzing clinical trends and ensuring adherence to current coding guidelines and industry standards set by regulatory bodies. |