Optimizing payment integrity for emergency department E/M claims
Jonathan Edwards | Cindy Kirby, M.D.

Evaluation and management (E/M) services serve as a fundamental component of the U.S. healthcare system, facilitating patient care across various settings, including emergency departments, hospital inpatient units, office visits, home services, and telehealth. Given the high volume of services and the complex criteria used to determine visit levels, E/M claims present a challenge for payers in maintaining payment integrity, particularly when it comes to appropriately coding emergency department (ED) claims, which can be a difficult issue between payers and providers. Improperly coded ED E/M claims can also negatively impact consumers directly, eroding the member’s plan benefits and resulting in higher out-of-pocket costs, plus time and frustration in trying to correct the improper bill.
What exacerbates confusion even further is that when patients seek care in the emergency department, charges are billed from two different sources. The ED provider will bill for the professional services rendered, while the facility where care is provided will bill for facility-related services such as imaging, lab work, and additional support team members.
A KFF analysis found that facility fees grew at four times the rate of professional fees for ED E/M services over several years.
In this white paper, we explore three key trends shaping emergency department (ED) E/M claims and examine their impact on payers and payment integrity programs. These findings are derived from claims analysis of a segment of Cotiviti’s Payment Policy Management database, encompassing more than 120 million covered lives. ED E/M claims refer to the specific Current Procedural Terminology (CPT) codes that healthcare providers use to document and bill for patient visits in the emergency department. These codes reflect the complexity and intensity of the services provided, directly influencing reimbursement and payment accuracy.
ED E/M utilization and unit costs are rising
Key findings reveal that E/M services represent a significant portion of ambulatory medical spending, accounting for up to 34% of total costs depending on the line of business (LOB). Within this category, emergency department services play a particularly influential role, making up as much as 22% of overall E/M expenditures and driving a substantial 75% of facility E/M costs. This highlights the critical impact of ED services on the broader healthcare spending landscape.
Between 2022 and 2024, ED E/M utilization, measured as claims per 1,000 members, grew at an annualized rate of 7% across all lines of business. The most significant growth in utilization occurred within the commercial and Medicare populations, with increases of 15% and 13%, respectively. In parallel with utilization growth, ED E/M unit costs, measured as paid per claim line, grew 5–9% depending on line of business. The growth in ED E/M utilization and unit cost underscores the impact of this area of spend on payers’ medical loss ratio (MLR).
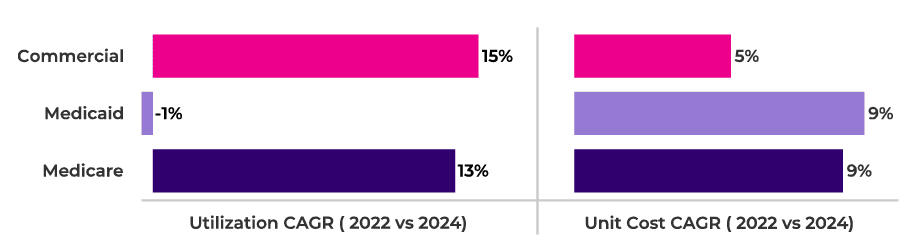
Figure 1. ED E/M utilization and unit cost growth by line of business.
In addition, spending patterns reveal a concentration of costs among a select group of conditions. The top 10 diagnosis groups accounted for approximately 45% of total ED E/M spending, emphasizing the outsized influence of specific medical conditions on overall emergency care expenditures. Further, despite increases in utilization, the diagnostic profile has remained largely consistent over three years, suggesting disease mix/patient acuity has not materially changed.
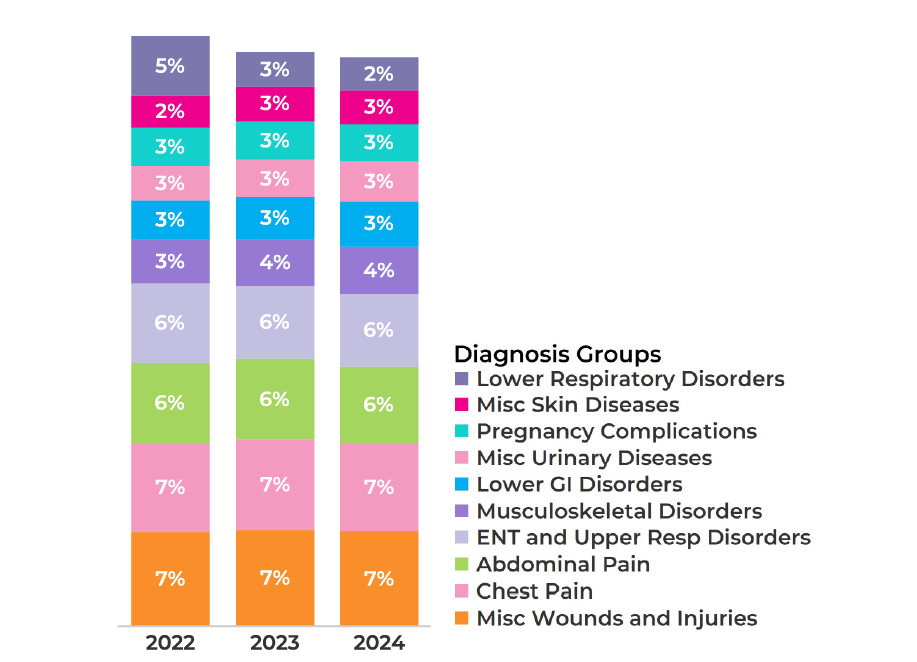
Figure 2. Distribution of ED E/M spend across top 10 diagnosis groups.
Use of high-level ED E/M codes continues to increase
The billing of high-level E/M codes (Levels 4 and 5) has continued to rise, even as the overall diagnosis profile has remained stable (see Figure 2). This trend suggests a shift in coding practices rather than a fundamental change in patient acuity, highlighting the evolving landscape of medical billing and documentation.
Between 2022 and 2024, the use of Level 4/5 E/M codes increased from 42% to 46%, reflecting a steady upward trajectory in high-level coding. Professional ED services experienced the most notable growth, with Level 4/5 coding surging from 71% in 2022 to 84% in 2024. This substantial rise underscores the increasing complexity of documentation and billing practices for physicians practicing within emergency care settings.
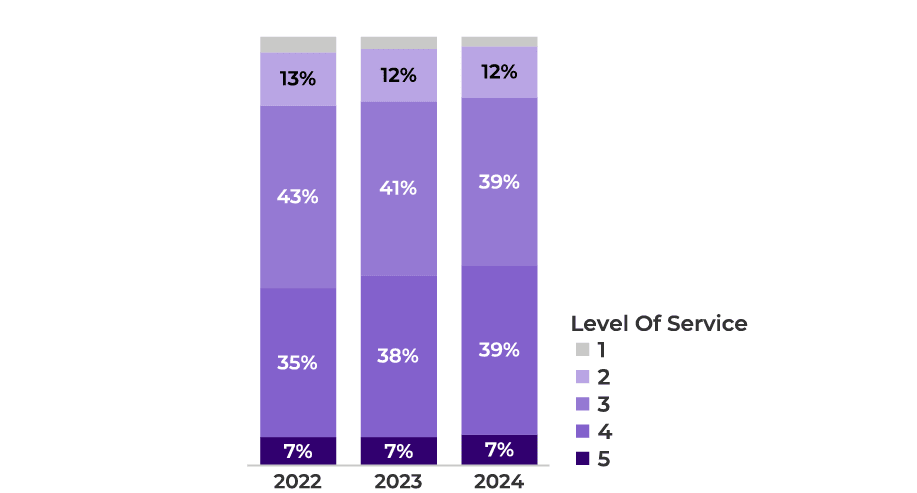
Figure 3. Distribution of E/M claim lines by level of service.
Cotiviti analysis indicates this trend is consistent across all regions of the country, indicating a broad industry-wide shift rather than a localized phenomenon. One key factor contributing to this increase is the widespread adoption of electronic medical records (EMR), which has streamlined the ability to meet high-level coding requirements. Many EMR systems even suggest coding levels to the provider based on level of documentation. As EMR systems continue to enhance documentation efficiency, providers are better equipped to justify higher-level codes, further driving this trend in medical billing.
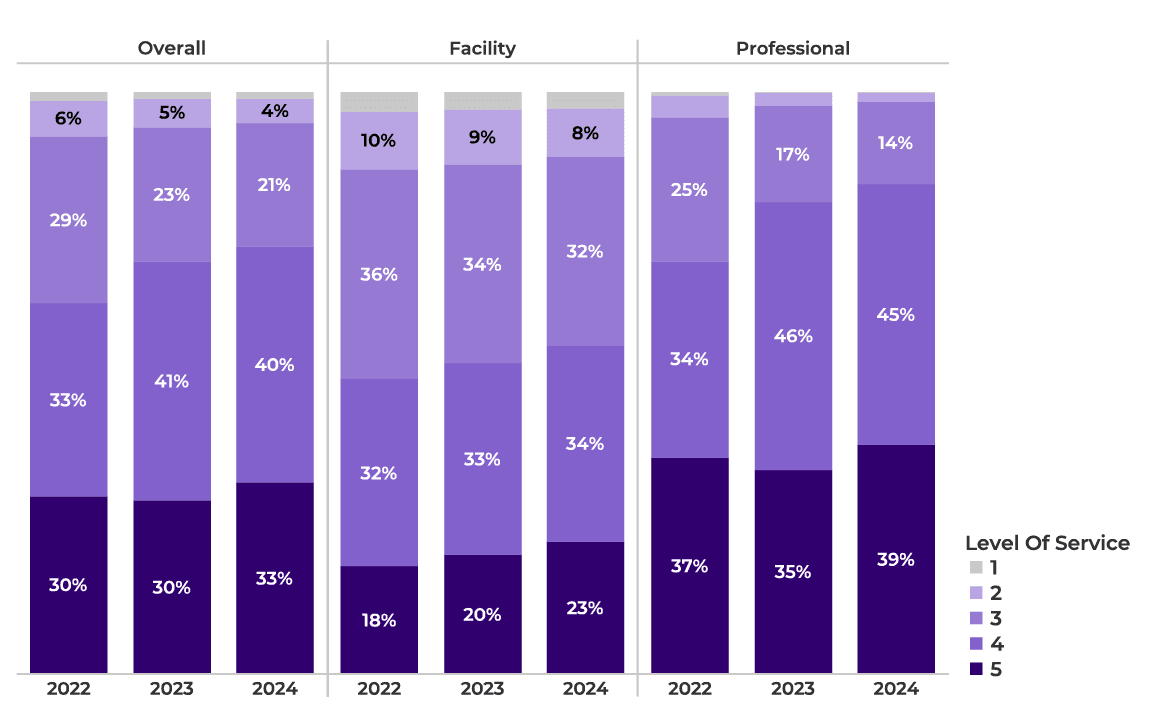
Figure 4. Distribution of ED E/M claim lines by level of service.
Cotiviti clients are capturing payment errors for ED E/M services
As health plans continue to refine their payment integrity strategies, there has been a noticeable shift toward addressing over-coding in ED E/M claims. These efforts aim to ensure that coding accurately reflects the complexity of care provided, ultimately reducing unnecessary costs, improving billing accuracy, and protecting plan members from undue financial burden and frustration.
An increase in high-level ED E/M claims by itself does not indicate any wrongdoing on the part of providers. However, when we observe a subsequent rise in ED E/M over-coding edits firing, it signals a growing trend of improper claim submissions. Between 2022 and 2024, the medical cost savings rate on ED E/M claims increased by 25%, rising from 0.8% to 1.0%. This increase in medical cost savings corresponded with an 18% annualized increase in claim editing rates on ED E/M claims. The most significant impact was observed in professional claims, where over-coding payment policies played a key role in driving cost containment. These policies assess diagnosis complexity to determine the appropriate E/M coding level, helping to curb excessive billing.
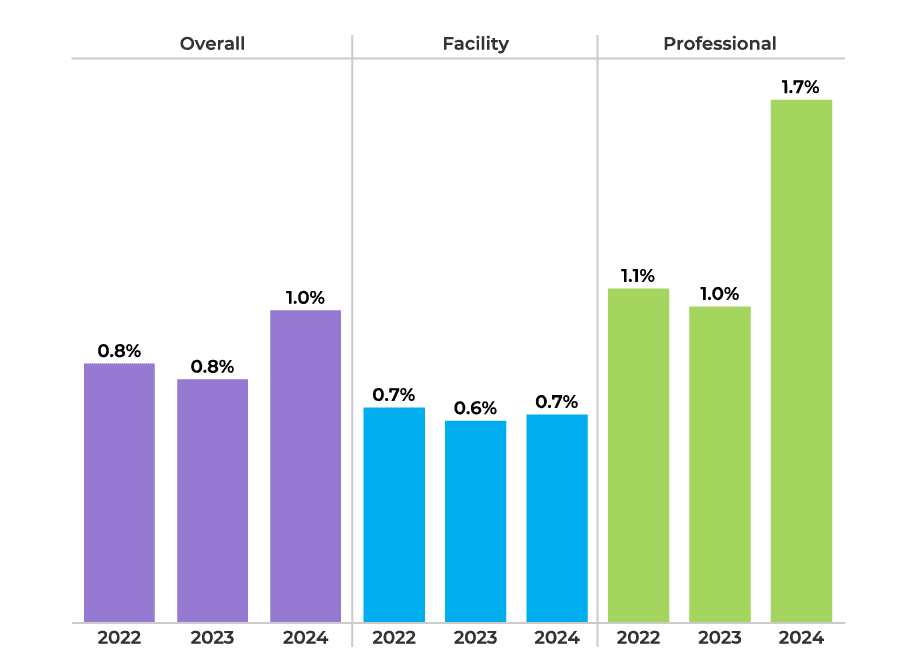
Figure 5. Medical cost savings rate on ED E/M claims.
A growing body of data highlights the prevalence of over-coding, and Cotiviti’s analysis illustrates that more than 40% of professional providers upcode at least half of their ED E/M services. In response, over-coding policies accounted for 65% of total ED E/M payment integrity savings in 2024, reinforcing their effectiveness in containing inappropriate costs.
On the facility side, similar scrutiny is being applied, with over-coding policies evaluating resource utilization—such as laboratory tests, IV fluids, and imaging—to ensure that E/M levels align with the actual intensity of care provided. As payment integrity measures continue to evolve, health plans are increasingly leveraging data-driven approaches to enhance coding accuracy and promote more sustainable healthcare spending.
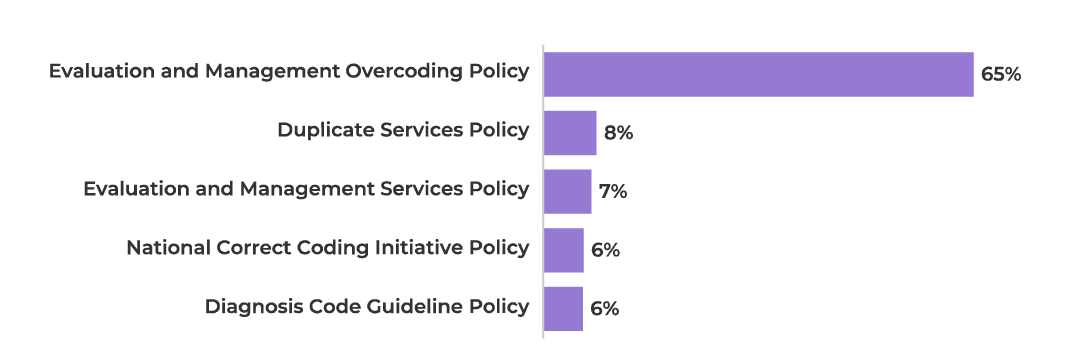
Figure 6. Distribution of ED E/M payment integrity savings by medical policy.
Leveraging data-driven insights for payment integrity
The increasing use of high-level E/M codes underscores the need for effective payment integrity measures. Cotiviti’s over-coding policies play a critical role in curbing excessive billing and ensuring accurate payment for ED E/M services. Health plans can further improve accuracy by extending payment integrity policies to facility ED claims, reinforcing the value of robust claim review programs.
By monitoring these trends and applying data-driven payment integrity strategies, payers can better manage medical costs and ensure appropriate reimbursement for emergency services—ultimately enabling them to better serve their members.
How to perform beyond expectations in payment integrity
Cotiviti’s Payment Policy Management solution enables payers to make informed, data-driven, clinically centered decisions on payment policy in numerous areas including E/M. Learn more about how our clinical, technical and service advantages make Payment Policy Management the leading final-filter editing solution for payers.
Start the conversation
We’re ready to help you understand how E/M coding trends are impacting your claims and your members. Request a conversation with our team and learn how we can perform an opportunity analysis to see what value you could achieve with Cotiviti.
About the authors
|
|
Jonathan Edwards Jon leads a talented team of analytic professionals that deliver actionable insights powering Cotiviti’s most important growth opportunities. With more than 15 years of healthcare analytics and consulting experience, Jon harnesses the power of data to develop leading-class analytic products and services that inform decision-making, accelerate growth, and differentiate Cotiviti’s value proposition. |
 |
Cindy Kirby, M.D. Dr. Kirby is responsible for helping Cotiviti's payer clients optimize the value they achieve from Cotiviti's Payment Accuracy solutions by understanding and implementing new payment policies. Prior to joining Cotiviti in 2018, she spent several years serving as a medical director for Humana, working in the southeastern regional market and later in fraud, waste, and abuse. |