Fill form to unlock content
Error - something went wrong!
Please complete this brief form to read this white paper.
Thank you!
Prepay integrity: What the self-insurance industry needs to know

Self-insured employers are managing a greater amount of the commercial covered population. As healthcare costs continue to grow and challenges such as inappropriate coding or waste and abuse persist, health plans are experiencing an increase in inappropriate medical spend. Similarly, rising medical costs for self-funded employers is causing them to look more closely at the payment integrity measures implemented by their third-party administrators (TPA).
According to the Kaiser Family Foundation, 65% of covered workers belonged to a self-funded health plan in 2023. For large firms (200+ workers), that figure jumps to 82%, and for the largest companies with 5,000+ employees, it soars to 93%. In addition, the Society of Professional Benefit Administrators observed that self-funding has grown so popular that many payers “are offering self-funding as their primary product.” Therefore, administering a high-performing payment integrity program along with the other services that support self-insured employers is more important for TPAs than ever.
What is payment integrity?
Payment integrity is the process of ensuring that healthcare claims are paid appropriately and accurately—without delaying payments to healthcare providers. Payment integrity solutions encompass both prepay solutions, which analyze claims before they are paid to prevent inappropriate payments, and postpay solutions, which analyze claims after they are paid to pursue overpayment recoveries.
The bedrock of prepay integrity solutions are automated claim editing systems, which rapidly analyze claims and determine whether they comply with internal payment policies as well as nationally sourced guidelines from agencies such as the Centers for Medicare & Medicaid Services (CMS) and organizations such as the American Medical Association (AMA). It’s not uncommon for medical plan sponsors, including self-insured employers, to have multiple claim editing systems in place (e.g., first- and second-pass) to prevent inappropriate claims from slipping through the cracks and getting paid. Indeed, based on Cotiviti’s own experience, payers without a second-pass editor in place may be missing out on millions of dollars in payment integrity savings each year.
Administering a high-performing payment integrity program along with the other services that support self-insured employers is more important for TPAs than ever.
Automated claim editing can also be complemented by manual prepay review of more complex coding scenarios, which typically can be performed without the burdensome process of requesting medical records from the provider. This creates a second line of defense against coding errors that can’t be caught by purely automated systems.
While postpay solutions are vital to analyzing the most complex claim scenarios, payers gain the most benefit from preventing inappropriate payments from occurring in the first place whenever possible. This is because pursuing overpayment recovery is not only less efficient and increases administrative burden, but can also cause friction with providers.
Why is prepay integrity important for TPAs?
TPAs that do not offer prepay integrity services to self-funded employers risk the possibility of losing a competitive advantage. In fact, according to Cotiviti data, 74% of Cotiviti health plan clients with self-funded business are already integrating prepay final filter editing with self-insured employers. Implementing payment integrity efforts with self-funded employers can help administering TPAs improve client retention and satisfaction and keep employee out-of-pocket costs in check.
All self-insured employers have a fiduciary responsibility to make sure employees get the best care at the best price. Therefore, they are rightfully concerned with protecting the member benefit to find substantial medical cost savings with low administrative effort. A strong payment integrity program can help to provide just that. Within our own Cotiviti data, we’ve found that self-insured employers can save up to 4% in annual professional and institutional claim costs with Cotiviti’s prepay integrity solutions, Payment Policy Management and Coding Validation.
TPAs themselves typically do not possess payment integrity capabilities, so they must contract with a vendor. To get started, TPAs must consider how to roll out a strategy, gaining the buy-in of self-funded employer clients. In this white paper, we will walk through the core steps: program design, contracting, employer engagement, and best practices in selecting a payment integrity partner.
Program design and contracting
Adding prepay integrity services should start right at the beginning of the TPA-employer relationship. Administering TPAs should consider providing it as a value-add as part of a standard package of services during the contracting phase of a new client acquisition, adding payment integrity shared services language to the contract to facilitate. This not only enables the employer to benefit from payment integrity efforts from the outset, but provides value to the TPA as well. Pass-through fees are easier to operationalize, and incremental savings can also provide a more competitive product for the TPA by creating a better unit cost structure, which is a great selling feature and good for retention.
There are two general ways to add payment integrity into an employer contract: opt-out or opt-in.
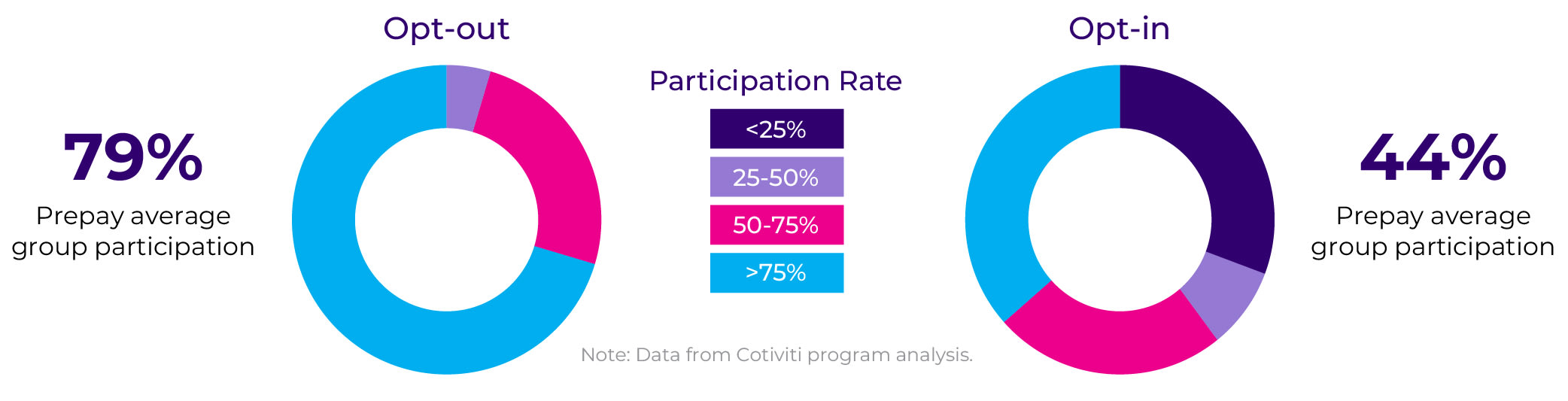
The opt-out model requires shared services to be added to the contract typically as a payment integrity shared service. Shared services are usually contracted in a way that allows TPA clients of the payment integrity vendor to pass through vendor fees. In an opt-out model, employers will typically have payment integrity programs added at their yearly renewal and will have to “opt out” of the additional savings and additional cost. Due to the nature of opt-out, clients typically keep payment integrity turned on as they see the value of the additional savings and there is a clear ROI. Opt-out also typically has a higher penetration rate. Among Cotiviti’s health plan clients with administrative services only (ASO) business, we see an average prepay participation rate of 79% for opt-out arrangements, compared with only 44% for those with opt-in (Figure 1).
Adding prepay integrity services should start right at the beginning of the TPA-employer relationship.
The opt-in model, by contrast, does not require shared services to be specified in the contract and is most likely contracted as a new or separate service line in the contract. In an opt-in model, the TPA is required to specifically contract with the employer to add this line item for extended payment integrity services. The opt-in model typically has lower volumes and lower penetration rates and is an extended timeline for penetration.
Figure 1. Opt-out participation rates vs. opt-in participation rates (click to enlarge).
Employer engagement
Educating self-insured employers about the benefits and roll-out process of prepay integrity solutions helps reinforce their value. Self-insured employer clients may need help understanding why payment integrity matters to their employees, why it’s worth it, the value of a payment accuracy policy specialist, and how contracting will work.
TPAs should consider positioning value in a few ways:
- Delineate services: Separate payment integrity from claims administration services
- Differentiate solutions: Distinguish between prepay and postpay solutions while emphasizing the immediate value of prepay solutions
- Mind timing: Engage with employers before contract renewal or open enrollment
Best practices in choosing a payment integrity partner
To demonstrate their full value, TPAs should show their plan sponsors that they are working with a best-practice payment integrity vendor as an extension of their services. Key qualities to look for in a potential partner include:
- Proven track record in prepay integrity. The vendor should be able to handle not only automated editing of standard claims, but also offer expert prepay review of more complex claim scenarios. Vendors that are only able to offer postpay analysis of complex claims will require the plan sponsor to pursue more costly and abrasive overpayment recoveries and will generally realize lower medical cost savings.
- Offering provider education within your leased network. If your providers are unfamiliar with payment integrity vendors and are not used to managing their edits and prepay reviews, implementing such a solution will be more likely to increase provider friction with the plan sponsor. An effective means to introduce payment integrity to the provider network is through notification and communicating the demonstrated value of your selected vendor, including the tools they offer for providers to check on the payment status of their claims and understand why they may have been modified or denied.
- Comprehensive and continuously updated payment integrity content. From specialty pharmacy to inpatient to ambulance claims and more, your vendor should have payment integrity policies in place to cover every claim scenario. Equally important, your vendor should take on the responsibility of updating these policies according to the latest rules and guidelines, rather than letting that burden fall on the TPA or plan sponsor.
- Ability to support provider appeals. While a strong payment integrity solution will minimize the number of payment decisions appealed by providers, appeals are an inevitable part of payment integrity. Your vendor should support appeals with inquiry tools, appeal support models, and guidance that can rapidly justify a payment decision on each claim.
- SaaS model with robust reporting and clinical support. A SaaS model enables the vendor to continuously deploy updates versus requiring the TPA to do so. Having clinical experts on staff and robust reporting are also crucial to offer the TPA and plan sponsor guidance and support through the process of policy selection, assessment, customization, and maintenance.
The vendor should be able to handle not only automated editing of standard claims, but also offer expert prepay review of more complex claim scenarios.
While implementing payment integrity efforts for self-funded plan sponsors can seem daunting, gaining a competitive advantage and maintaining a good working relationship with self-insured employers makes it worth it. Rolling out the right strategy and the right employer engagement plan can make all the difference. By taking a thoughtful approach, TPAs can extend savings to self-insured employers and simultaneously help their standing in the marketplace.
To learn the possibilities with your own self-insured employer clients, explore Cotiviti’s prepay solutions for TPAs and see how to:
- Avoid payment errors before claims are paid
- Lower administrative costs by reducing “pay and chase”
- Maintain positive provider relationships while ensuring payment integrity
Looking to dig deeper?
Contact our experts today to learn about how Cotiviti can help.