CMS Star Ratings: A guide to quality improvement

Quality regulations have been at the forefront of healthcare for the past few decades, keeping health plans accountable for helping members get the best level of care. Landmark quality measures like the Centers for Medicare & Medicaid Services (CMS) Star Ratings and the National Committee for Quality Assurance (NCQA) Healthcare Effectiveness Data and Information Set (HEDIS®) are central to these efforts, helping plans to get better assessments of care and areas where they can improve. In performing well across these quality measures, plans have the chance to improve health outcomes, prove the quality of their networks against the competition, and even earn back revenue to incentivize continued excellence.
Star Ratings have been in place for decades as one of the core quality measure sets for health plans participating in the Medicare Advantage and Part D Prescription Drug programs. As a crucial element of quality improvement efforts, health plans can benefit from understanding Star Ratings methodology and history and learning best practices for improving year over year. Plans that prioritize understanding the ins and outs of Star Ratings are also incentivized by CMS with substantial bonus payments for high ratings.
Read on to learn about CMS’s Star Ratings quality rating system, how it works, and different ways your plan can improve your own Star Ratings for better quality of care.
Table of contents
CMS Star Ratings and methodology changes
The most recent changes to CMS Star Ratings
Best practices for better CMS Star Ratings
What are CMS Star Ratings?
The CMS Star Ratings system began in 2007 as part of the Medicare Advantage and Part D Prescription Drug programs. This five-star quality rating system measures the experiences that Medicare beneficiaries have with the health plan and the healthcare system overall and was started as a way to give health plan members a straightforward way to judge the quality of their plans.
Per the Star Ratings methodology, plans are rated on a scale between one and five stars, with one star being the lowest quality rating and five stars being the highest. After the plan has been assessed by CMS, the resultant rating is published on the Medicare website. Doing so is meant to improve overall quality of care across Medicare beneficiaries, the overall networks themselves, and also helps members to compare plans during Open Enrollment with a level of transparency. Plans benefit from clear feedback about the overall quality of care, which includes the incentive of rewards for outstanding care and the threat of penalties for neglect.
Plans that score high Star Ratings are rewarded with significant bonuses that reflect the success of their plans in meeting member needs. Plans that receive these bonuses often use them to fund supplemental benefits for even further improvements, and additional revenue can have significant impact on medical loss ratio (MLR). CMS is projected to spend $15 billion on Medicare Advantage quality bonus payments.
Another key factor in Star Ratings is the changes to their methodology each year. Since population health, medical trends, and numerous other factors impact approaches to care each year, Star Ratings morph with the times. For example, methodologies for cut points can vary, different procedures can be weighed differently, and even different provisions or revisions can be made each year to correct years previous. Health plans eagerly await news of updates each year to ensure that they can match the most current set of rules for Star Ratings.
CMS Star Ratings program and methodology changes
Some of the largest Star Ratings changes in recent years include the continual adjustment for cut points to determine ratings, the statistical methodology for calculating those cut points, the changes to measure weights each year, and added provisions like the Hold Harmless provision.
Star Ratings cut point methodology
Star Ratings are determined by a cut point methodology, a process of setting the point thresholds or “cut points” for each Star Rating score. These defined cut points determine the level of performance required to achieve a particular rating and are subject to change as CMS deems fit.
A significant change that was put in place for the 2022 Star Ratings year introduced mean resampling to reduce the sensitivity of the clustering algorithm used to create the cut points to outliers. This change was meant to stabilize cut points. For 2024, CMS took this a step further by introducing the Tukey outlier methodology to remove exceptionally high and low scores compared to the rest of the industry. This change aimed to eliminate outliers and provide a fairer representation of a plan's performance. However, CMS was challenged to re-calculate the 2024 Star Ratings due to court rulings on lawsuits from SCAN Health Plan and Elevance Health. The lawsuits alleged that Medicare Advantage plans were not given proper notifications of changes to the Tukey outlier statistical model for calculating cut points.
CMS is trying to meet the need for a more dynamic and responsive methodology that accurately reflects large shifts in the industry’s performance. For example, many plans saw a drop in preventative screenings during the COVID-19 pandemic, but guardrails prevented the cut points from fully reflecting the market’s drop in those rates. A recent proposal suggests the removal of guardrails for non-CAHPS® measures. This change would allow for more significant shifts in cut points exceeding 5%, which can have a significant impact on a plan’s overall score.
Star Ratings measure weight changes
Another key piece of the Star Ratings program that changes frequently is the weighting of each measure and measure category. These changes impact the contributions of different measures to the overall Star Ratings. For example, for the 2024 Star Ratings, CMS proposed an increase in weight attributed to pharmacy contributions. This change signified a heavier emphasis on monitoring and measuring pharmacy-related outcomes. Weight changes in the past few years have indicated a shift towards being more quantitative rather than solely qualitative, including health equity and additional pharmacy measures focusing on outcomes.
For the 2026 Star Ratings, CMS decreased the weight of Patient Experience/Complaints and Access measures from 4x to 2x—meaning that 16 measures are set to lose half their weight. This is significant as MA plans have invested time and resources into these qualitative measures in the past several years, prompted by their prior increase in weight from 1x to 4x, only to see their weight decrease once more.
See Figure 1 below for further evidence of the shifting weights of Star Ratings, as well as other regulatory measures. This graph shows how the program has changed over the last several years, with some categories, such as HEDIS measures, increasing in relative importance and others such as Operations decreasing.
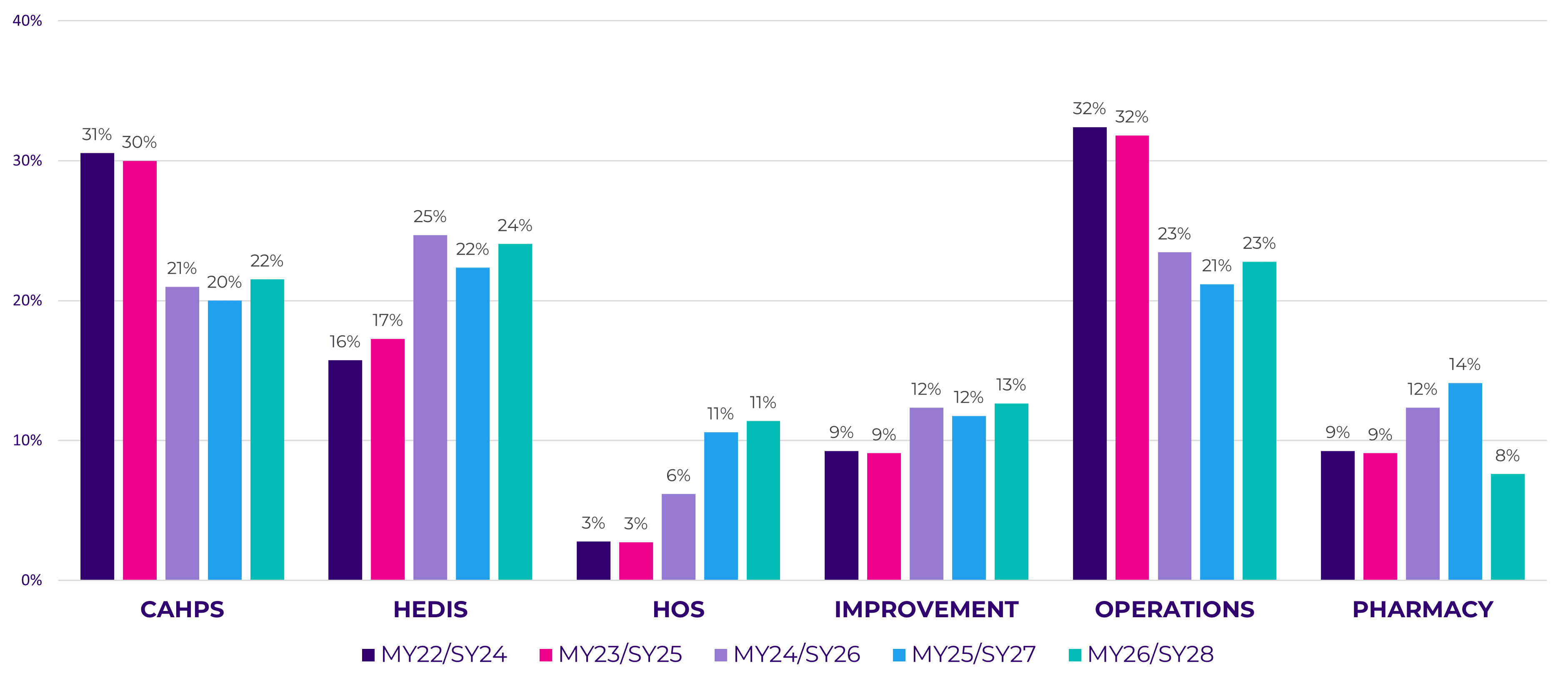
Figure 1. Changes in weighted category contributions towards overall Star Ratings from 2024–2028 Star Ratings years.
While changes like this can be disruptive, they also offer an opportunity for plans to shift focus and keep up with trends relevant to care for the current population.
Star Ratings Hold Harmless provision
The Hold Harmless provision is another notable change that impacts Star Ratings. Initially introduced in 2018, its original intent was to recognize that higher performing contracts have less room for improvement. Therefore, a health plan’s overall rating was calculated both with and without the Health Plan Quality Improvement and Drug Plan Quality Improvement measures. Contracts achieving four stars or more were held harmless from having their rating reduced by the inclusion of these measures.
However, CMS stated “our experience with the Part C and Part D Star Ratings program since this policy was finalized suggests that contracts with 4 or 4.5 stars for their highest rating still have room for improvement.” Therefore, the agency has adjusted the provision for the 2026 Star Ratings year by only allowing five-star plans to apply the provision.
CMS estimates that this change to the Hold Harmless threshold will result in a 10-year Medicare savings exceeding $19.3 billion. This will make it harder for high-performing plans to achieve and maintain even higher Star Ratings.
Learn the latest updates and changes to Star Ratings measures for the upcoming year with our Cotiviti Star Ratings calendar.
The most recent changes to CMS Star Ratings
While cut points, measure weights, and landmark provisions are some of the most expected changes each year, every year is different. Take a look at some of the other recent methodology changes from the past several years:
- The scaled reduction approach (2020 Star Ratings): Before 2019, CMS automatically reduced a plan’s measure rating to one star if it determined that the measure data was “incomplete, biased, or erroneous.” However, in 2019 it implemented a system called “scaled reductions.” Rather than a one-size-fits-all approach that automatically reduced a plan to one star when CMS found the data to be incomplete, biased, or erroneous, the plan’s Star Rating would be reduced one star at a time based on the degree of data accuracy. This meant that a plan with more missing independent review entity (IRE) data would see a greater reduction than a plan with a lower degree of missing data.
- The COVID-19 pandemic (2021 Star Ratings): As healthcare organizations grappled with the onset of the COVID-19 pandemic, CMS took two major actions to try to offset long-ranging effects on the Medicare Advantage Star Ratings Program. When the agency released its Contract Year 2021 Medicare Advantage and Part D Final Rule, it changed Star Rating cut points and shifted greater emphasis to patient experience while adding more significance to access measures. Through the Interim Final Rule, CMS took another large step in reforming star ratings to account for the effects of the coronavirus pandemic, suspending reporting requirements for Star Ratings in 2020 and letting CMS to continue to use providers’ scores from the previous year.
- Continued impacts of COVID-19 (2022 Star Ratings): To account for changes in care brought on by the COVID-19 pandemic, CMS implemented several changes for Star Ratings 2022, including:
- The use of “better of” methodology: This change allowed plans to count data from either the 2021 or 2022 Star Ratings, giving them the benefit of choosing a previous year with better data.
- CAHPS member experience: CAHPS changed the relative weighting of patient experience measures. For the 2021 Star Ratings, the weight changed from a 1.5x to 2x, increasing yet again in 2023 to 4x, thus placing more emphasis on member experience over outcomes.
- Removal of 3x-weighted HOS measures: Due to COVID-19 impacts, CMS elected to remove Improving/Maintaining Physical Health and Improving/Maintaining Mental Health measures from the calculation, providing a boost to most plans’ ratings.
- The fallout from lifted COVID-19 measures (2023 Star Ratings): When CMS released the 2023 Star Ratings, the concerns of many Medicare Advantage (MA) plans were realized as overall ratings declined across the industry. As a result of lifting most of the guardrails implemented at the COVID-19 pandemic lifted, the average Star Rating dipped from 4.37 to 4.15 when weighted by enrollment. According to Cotiviti data, the number of MA contracts earning a 4-star rating or higher dipped from 68% for the 2022 Star Ratings to just 51% for the 2023 Star Ratings.
- The Tukey outlier deletion model (2024 Star Ratings): As anticipated by the healthcare industry, the 2024 Star Ratings demonstrated an overall decline in health plan performance for the second consecutive year. With several significant changes such as the implementation of the Tukey outlier deletion model, measure weight changes, and the Hold Harmless provision. According to Cotiviti data, the average rating for Medicare Advantage plans with prescription drug coverage (MA-PD) dropped from 4.14 to 4.04 when weighted by enrollment. Furthermore, the percentage of MA-PD contracts earning four stars or higher dropped from 51% for the 2023 Star Ratings to just 42% for the 2024 Star Ratings. As previously mentioned, this methodology change is being reassessed after CMS was sued.
- EHO4all (2027 Star Ratings): CMS originally introduced the Health Equity Index (HEI) to the 2027 Star Ratings program to reward Medicare Advantage plans that provide high-quality care to underserved populations, including those with low income, dual eligibility, and disabilities. It was then renamed to Excellent Health Outcomes for All (EHO4all) in the 2026 Final Rate Announcement. EHO4all aims to shift how plans receive performance bonuses, potentially leading to some gaining or losing up to half a star, and is expected to save $5.12 billion over 10 years.
Best practices for better CMS Star Ratings
Successfully navigating changes in Star Rating programs requires a proactive approach and the implementation of key interventions to bolster ratings, improve member experience, and ease provider relations. To enhance your success in navigating changes in Star Rating programs, consider implementing the following steps.
Create a baseline
Establishing a baseline is essential to understand your plan's current performance and identify areas for improvement. Start by conducting a comprehensive assessment of your plan's performance across different measures included in the Star Ratings program. This assessment will help you understand your strengths and weaknesses and provide a clear picture of where you stand in relation to the desired Star Ratings. Analyze your performance data, such as healthcare outcomes, member satisfaction scores, and adherence to clinical guidelines.
This baseline assessment will serve as a reference point for tracking progress and measuring the impact of your improvement efforts. Benchmark your performance against industry averages and top-performing plans to gain insights into areas where you may be lagging.
Evaluate against predicted cut points
As Star Rating programs evolve, so do the cut point methodologies used to determine Star Ratings. It is crucial to assess how changes in cut point methodologies may impact your plan's ratings. Utilize historical data and industry trends to predict potential cut point changes and evaluate your performance against these predicted points. This is also an area where technology is a considerable support. Predictive cut point modeling takes the guesswork out of having to track cut point methodology changes manually.
By conducting this evaluation, you can identify areas where your plan may fall short and proactively develop strategies to improve your performance. Focus on measures that have a significant impact on Star Ratings and align your improvement efforts accordingly. Prioritize measures that contribute the most to your overall ratings to maximize your chances of achieving higher Star Ratings.
Prioritize performance improvement with both prospective and retrospective tactics
Once you have identified the measures that have the most considerable influence on your Star Ratings, it's time to develop targeted strategies for performance improvement. Consider implementing initiatives that address specific areas of improvement, such as clinical outcomes, member experience, preventive care, and care coordination.
A key step is engaging stakeholders, including providers, care teams, and administrative staff, to collaborate on quality improvement initiatives. By leveraging their expertise and insights and inviting them in, you can gain valuable perspectives and innovative ideas to enhance your performance in star rating programs. Ask them for the resources, infrastructure, and training programs they need to support performance improvement efforts.
Leverage data analytics and performance management tools to monitor performance, track progress, and identify areas that require further enhancement. You should regularly review your performance metrics and adjust your strategies as needed to ensure continuous improvement.
Throughout this process, you must provide your staff with the necessary tools and knowledge to deliver high-quality care consistently. And to ensure buy-in, foster a culture of quality and accountability within your organization, emphasizing the importance of meeting and exceeding performance targets.
Engage with members and providers
Engaging with your members and providers is crucial for achieving improved Star Ratings. Strong relationships with both parties can lead to better health outcomes, increased member satisfaction, and improved adherence to preventive care measures.
First, you will want to develop and implement strategies to actively engage members in their healthcare journey. A good place to start is with educational materials, personalized communication, and tools to help members make informed decisions about their health. With these resources and your outreach, you should encourage members to participate in health and wellness programs, preventive screenings, and care management initiatives. And don’t be afraid to actively seek feedback from members to understand their needs and preferences and use that information to tailor your services accordingly.
To connect with providers, begin by collaborating closely with them to improve care coordination and delivery. Work with them to implement care management protocols, establish regular communication channels, and promote evidence-based practices. Throughout this process, engage providers in quality improvement activities, such as peer learning and sharing best practices. And provide them with timely and actionable performance data to help them identify areas for improvement and track their progress. By actively involving members and providers in your quality improvement efforts, you can create a collaborative healthcare ecosystem that drives better outcomes and contributes to higher Star Ratings.
Remember, successfully navigating changes in Star Ratings programs requires a proactive and data-driven approach. Continuously monitor industry updates, stay informed about changes in methodologies, and adapt your strategies accordingly. By prioritizing performance improvement, engaging stakeholders, and leveraging data and analytics, you can enhance your plan's success in achieving higher Star Ratings and delivering exceptional care to your members.
How to close quality care gaps
A specific area of focus for improving quality scores is closing gaps in care, especially as the weighted category contribution of HEDIS measures towards overall Star Ratings increases.
Consider some of the following strategies to reach your target Star Rating and reduce care gaps:
- Use one vendor for HEDIS measurement, Star Rating tracking and prediction, and member engagement to help with consistency and gap closure across all measures while reducing member abrasion. Bringing efforts together can ensure a more seamless member experience.
- Review the previous years’ performance and compare it against simulated cut points. Identify whether any measures will fall short of the rating received from the previous year or if you are projected to miss your target for the next year. Even a one-point difference can reduce your measure rating from four to three stars.
- Gain a clear view of progress with trending and benchmarking dashboards by leveraging advanced analytics that offer measure predictions, trends, and opportunities for growth.
Some measures are more relevant to a particular plan than others for Star Ratings. Let’s examine some of the focus areas that Star Ratings measures for improvement.
Heart disease
Heart disease is the leading cause of death in the United States, accounting for nearly 700,000 deaths each year. Its chief risk factor is high blood pressure or hypertension, which not only increases the risk of cardiovascular disease (CVD) including heart attack and stroke, but also kidney disease and other conditions. Known as the “silent killer,” CVD affects an estimated 121.5 million Americans, with a heart attack occurring approximately every 40 seconds according to the Centers for Disease Control and Prevention (CDC). Although men are more likely to suffer from CVD, other major risk factors include age, heredity, and stress. With proactive care and observance of a low-sodium diet, physical activity, and consistent medication adherence for those with CVD, these conditions can be managed and lower the risk of a heart attack.
Both NCQA and CMS have recognized that quality care standards are critical for plans to follow to support members’ cardiovascular health, which includes monitoring a number of related measures in both the HEDIS® and Star Ratings programs.
The Star Ratings measures related to heart conditions included Controlling High Blood Pressure (CBP), Statin Therapy for Patients with Cardiovascular Disease (SPC), Medication Adherence for Hypertension (ADH), and Medication Adherence for Cholesterol (MAC). With the exception of SPC, each of these measures carried a weight of 3x, demonstrating CMS’s increased focus on measures related to cardiovascular health.
Plan ahead for the next Star Ratings by focusing on personalized messaging to deliver information to members at the right time and inspire action to reduce the effects of CVD. Early care gap closure is possible when effective member engagement interventions are in place.
Colorectal cancer
Treatment for colorectal cancer in its earliest stage can lead to a 90% survival rate after five years. However, more than a quarter of adults ages 50–75 are not up to date on their recommended screenings, a problem that was only exacerbated by the COVID-19 pandemic. One simulated model estimated that the number of colorectal cancer screenings nationwide decreased by as much as 2 million due to the pandemic and led to thousands of missed early-stage diagnoses.
Prevention is crucial to mitigating the number of people who experience terminal colorectal cancer. Adults ages 45–75 are now urged to get a colorectal cancer screening, following a May 2021 update by the U.S. Preventive Services Task Force (USPSTF) lowering the recommended screening age to 45 from 50. Colorectal cancer can be screened through numerous methods including colonoscopy, virtual colonoscopy using computed tomography, fecal occult blood test (FOBT), sigmoidoscopy, and DNA stool test. There are even options for home testing, such as a fecal immunochemical tests (FIT).
As these guidelines evolve, health plans must be aware of important changes to their quality measurement programs like Star Ratings:
- For the 2025 Star Ratings, previously optional exclusions for the COL measure became required exclusions.
- An increase in scores for contracts at the lower end of the distribution for COL pushed cut points higher in the 2025 Star Ratings
Below are strategies plans should consider to optimize their quality scores while improving the health of their member population:
- Offer multiple screening options. Make members aware that home testing options such as FITs and other alternatives to a colonoscopy are available. One study found that only 38% of participants who had just a colonoscopy recommended completed their screening, compared to 67.2% who were recommended an FOBT and 68.8% who were given a choice between a colonoscopy or FOBT. Educating members on all the available options increases the likelihood of screening and catching cancer sooner.
- Deploy tailored communications instead of a single message. As noted in one 2022 study, “a key challenge in developing cancer screening messages is ensuring that patients perceive information about their cancer risk as personally relevant.” Researchers found that sending targeted messages to participants increased their intention to be screened for colorectal cancer. This is also reflected in Cotiviti’s own client data. Members who received targeted communications about colorectal cancer screening through the Eliza consumer engagement solution had a 4.3% higher rate of gap closure than those who were unengaged.
- Collaborate with providers and your IT department to prepare for the ECDS transition. Save chart review results in your HEDIS reporting tool to use as supplemental data and bring your internal IT stakeholders together to create a repository to house historical colorectal cancer screenings. This ensures future access to this valuable data. Work together externally with providers to gain historical data on members, helping to select the right metrics, benchmarks, and reporting to engage them in closing care gaps.
Remember why this ultimately matters: Early treatment for colorectal cancer leads to much higher survival rates. Through effective member and provider engagement, coupled with robust quality measurement and reporting tools, health plans can make a tangible impact to their members’ long-term health.
Cardiovascular health
Cardiovascular disease poses a significant health challenge for millions of Americans, with high or borderline-high cholesterol levels impacting nearly 35% of U.S. adults and serving as a significant contributing factor to heart disease. Perhaps most concerning is that high blood cholesterol typically has no signs or symptoms, necessitating regular testing for detection.
Despite advancements in cholesterol-lowering treatments such as statins, consistent medication usage remains a concern, with only just over half of those who would benefit from cholesterol medication currently taking it. Health plans can help address this pressing healthcare dilemma with improved member engagement and better outreach.
In the Star Ratings program, Medication Adherence for Cholesterol (Statins) is a triple-weighted measure that evaluates consistent adherence rates for prescribed medications. Ratings are assigned based on the percent of plan members with a cholesterol medication prescription, typically a statin, “who fill their prescription often enough to cover 80% or more of the time they are supposed to be taking the medication.” The medication adherence measures were developed by the Pharmacy Quality Alliance (PQA).
Improving the rates of Americans checking their cholesterol levels and adhering to treatment plans requires a multi-step approach. Educating members about preventive care from the start helps uncover opportunities for early interventions and allows for plans to determine where resources should be allocated for better health outcomes, higher quality scores, and improved Star Ratings. Plans should also consider lifestyle factors related to high cholesterol that can be impacted, such as diet, obesity, smoking, drinking alcohol, and exercise. Helping members make informed choices, such as consuming vegetables and whole grains while reducing saturated and trans fats, can play a pivotal role in lowering cholesterol. Understanding member demographics and identifying those most likely to be impacted by high cholesterol is another key factor. Once you know your members better, you can support them with culturally competent communications that they are more likely to respond to, thereby driving improvements in quality, HOS/CAHPS® survey results, and member outcomes.
Looking to the next year
Star Ratings is a crucial part of an overall quality strategy, but it’s also just one part of the overall puzzle. Health plans should focus on optimizing Star Ratings in line with HEDIS measures, and other regulations and compliance measures.
As value-based reimbursement becomes the standard, health plans should consider how these measures can contribute to other efforts to drive the purchase, delivery, and utilization of higher value healthcare. Collaborating more effectively with provider networks, with members, and with other functional teams within the plan itself can result in successfully managing members’ clinical and financial risks, making the most of limited internal resources, and staying compliant with industry requirements and regulations.
Looking to improve your Star Ratings? Get started with Star Intelligence to track, predict, and model CMS Star Ratings and more for improved quality.
About Cotiviti
Cotiviti enables healthcare organizations to deliver better care at lower cost through advanced technology and data analytics that improve the quality and sustainability of healthcare in the United States. Cotiviti’s solutions increase transparency and collaboration between payers and providers while empowering them to reduce medical and administrative costs, enable better health, improve claims payment efficiency, streamline operations, drive interoperability, and advance value-based care. Its customers serve the majority of U.S. healthcare consumers, providing coverage and care for over 300 million members and patients. Additionally, Cotiviti offers data management and recovery audit services to the retail sector to improve business outcomes. For more information, visit www.cotiviti.com.
HEDIS® is a registered trademark of the National Committee for Quality Assurance (NCQA).
CAHPS® is a registered trademark of the Agency for Healthcare Research and Quality (AHRQ).