Achieving Star Ratings success in the ECDS era

The landscape of Medicare Advantage (MA) Star Ratings is undergoing a dramatic transformation as the healthcare industry shifts toward digital measurement. With the National Committee for Quality Assurance (NCQA) phasing out hybrid HEDIS® measures between now and 2029, and introducing more electronic clinical data systems (ECDS) measures each year, MA plans now need to adapt their own strategies. The traditional safety net of retrospective chart reviews is diminishing, compelling organizations to rely more on real-time administrative and electronic health record (EHR) data to demonstrate quality performance.
In this eBook, we explore the implications of this pivotal shift, equipping MA plan leaders with the knowledge and tools needed to maintain—and even boost—their Star Ratings in the ECDS era while improving provider and member engagement, ultimately delivering better care.
Table of contents
Hybrid HEDIS measures are rapidly disappearing
Triple-weighted measures are at risk
Hybrid HEDIS measures are rapidly disappearing
The hybrid method of HEDIS measurement occurs when plans sample medical records after year-end to find undocumented services or readings. The retirement of hybrid reporting in calendar year 2030 means plans lose the safety net of manual chart review, and any gaps in claims or EHR data will directly lower measured performance. The Colorectal Cancer Screening (COL) measure was one of the first major MA measures to make the jump from hybrid to ECDS-only in Measurement Year (MY) 2024, and the industry saw a notable performance decline as a result. NCQA’s data showed hybrid COL rates were about 10% higher than purely ECDS rates for MA plans (Figure 1).
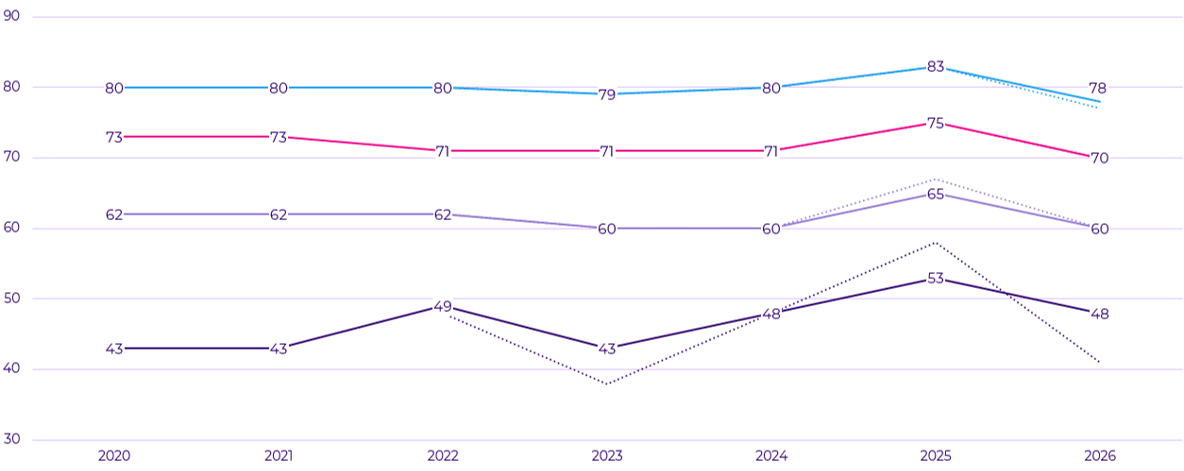
Figure 1. Cut points for the Colorectal Cancer Screening (COL) measure.
Eye Exam for Patients with Diabetes (EED) is one of the next measures to watch as it is facing retirement of hybrid reporting in MY 2025. Other current hybrid measures including Controlling High Blood Pressure (CBP), Care for Older Adults (COA), Transitions of Care (TRC), and Glycemic Status Assessment for Diabetes (GSD) will transition to ECDS in MY 2028 and MY 2029.
Plans that have been relying on chart chases each spring to find eye exam documentation will want to deploy new tactics immediately. As the 2026 Star Ratings result demonstrated, cut points for the COL measure plummeted by five points at the two-, three-, four-, and five-star levels, yet even this understates the true drop because of CMS guardrails, which prevented cut points from dropping even further. Many plans saw double-digit declines in their own COL results but still faced nearly the same four-star threshold due to the guardrail policy. This compressed plan ratings, giving MA plans a wake-up call that once-reliable hybrid lifts are vanishing.
Triple-weighted measures are at risk
It’s especially important for MA plans to consider HEDIS measures that carry greater weight in the Star Ratings program. In 2025, CMS weights most clinical outcomes measures at 3x, patient experience measures at 2x, and process measures at 1x.
In the HEDIS measure category, CBP, GSD, and Plan All-Cause Readmissions (PCR) account for a major portion of a plan’s Part C score, because each triple-weighted measure contributes as much to the summary rating as three individual single-weight measures. As these measures all transition to ECDS-only reporting, if plans don’t bolster their data-sharing and EHR integration now, they could face a severe hit when the change comes. Like COL, it’s not hard to imagine a similar 5–10 percentage point decline in CBP rates industry-wide when that measure loses hybrid collection—but with three times the impact.
On the Part D side, the three medication adherence measures—for diabetes, hypertension, and cholesterol medications—have historically been triple-weighted and collectively made up a large share of many plans’ overall Star score. CMS is introducing a health risk adjustment update to these adherence measures for MY 2026, treating them as “new” measures. As a result, in the 2028 Star Ratings, their weight will drop from 3x down to 1x. This temporary weight drop means Part D outcomes will carry far less influence in the overall rating, shifting even more relative weight onto Part C clinical measures.
Coupled with CAHPS® experience measures recently being scaled back from 4x to 2x weight for the 2026 Star Ratings, HEDIS clinical measures will soon dominate an MA plan’s overall Star Rating even more than today. Plans that perform best in adherence or patient surveys will no longer be able to rely on these measures carrying them to a high rating, and will want to refocus on clinical measures. Plans that fail to plan for ECDS will find themselves falling behind peers on these critical measures, and if low-rated contracts continue to consolidate or exit, the remaining cohort’s performance thresholds will only climb higher.
Year-round data strategy: Adapting to the ECDS era
The scramble of chasing charts after the measurement year ends is becoming a relic of the past. To thrive under ECDS, MA plans need to adopt a year-round, data-driven quality strategy. This means investing in processes and partnerships that continuously capture needed data before the measurement year closes. Here are key strategies to consider:
- Build robust clinical data exchange: Prioritize connectivity with providers via health information exchanges, FHIR APIs, and EHR integration. The goal is real-time or at least monthly data sharing of critical metrics (e.g., lab results, blood pressure readings, screening tests). By improving interoperability, plans can streamline quality reporting and minimize rating drops during ECDS transitions. Plans should treat clinical data as a strategic asset to ensure HEDIS vendor or internal systems can ingest and map electronic data to measure criteria.
- Engage providers with actionable gap reports and incentives: A year-round HEDIS mindset means providers shouldn’t be surprised by gaps in February—they should know in June who needs a screening. Good documentation is vital, ensuring providers record services and results in structured fields so that data isn’t lost. Consider embedding quality staff in high-volume provider offices or paying bonuses for hitting documentation targets.
- Leverage technology for smarter retrieval: When manual chart review is needed, make it as efficient as possible and don’t confine it to January through March. Use vendor tools to scour records for key data and to auto-abstract elements such as lab values. Plans are moving to continuous year-round medical record chart retrieval for select measures rather than one-time chases. This means if a member’s chart is pulled in July for a risk adjustment or care management review, any quality data (e.g., a nephropathy test result or a A1c test value) is captured and counted in HEDIS, rather than waiting to rediscover the same chart next spring.
- Audit your data and systems now: An often-overlooked aspect of ECDS readiness is ensuring your data pipeline is clean and complete. Use the HEDIS “off-season” to conduct a deep data quality audit. Work with your HEDIS auditor and IT team to verify that you’re properly capturing all claim codes, lab feeds, and supplemental files for each measure. Identify gaps where data might exist but isn’t flowing to your measurement engine. For instance, are you receiving COA medical review or functional status assessment data, or vision vendor data for eye exams? Fixing those now will pay dividends when hybrid reporting is retired. The more comprehensive your data, the closer your administrative/ECDS rate will approach what a full chart review might have found.
- Prospective outreach and member engagement: Don’t wait for measures to fail; proactively reach out to members who are due or overdue for services. Many plans now run off-season gap closure campaigns for things like cancer screenings and diabetic tests. The period after HEDIS submission is an ideal time to identify which measures and sub-populations underperformed and kick off interventions to improve those metrics in the current year. For example, if your COL screening rate missed the four-star mark, launch a campaign in summer or fall to engage those who haven’t completed a screening before the year is up. Use plan benefits such as transportation, at-home test kits, and free clinics to ease members’ burden. Year-round engagement also includes member education, such as sending reminders about why these screenings and tests are important to their health.
Don’t get caught unprepared
The transition from hybrid to ECDS reporting is a known shift that directly affects MA Star Ratings. Combined with rising cut point thresholds, a tougher scoring methodology, and the refocusing of weights onto clinical outcomes, this shift could accelerate the recent decline in Star Ratings across the industry. The good news is that plans still have time to adapt by strengthening their data infrastructure and quality improvement processes.
Don’t let the transition to ECDS catch your plan unable to pivot. Too many factors are already pushing Star Ratings down—with careful planning, this is one factor MA plans can control. By moving to a year-round, data-centric quality program, MA plans can maintain and even improve their measure rates without the crutch of retrospective chart reviews. Those that succeed will likely be the ones who treat interoperability and clinical data as strategic priorities today. In the end, the goal isn’t just to chase measures, but to truly integrate quality into care delivery in real-time. Plans that embrace this philosophy will not only protect their Star Ratings in the face of change, but also deliver better care for their members year-round.
Star Intelligence: A one-stop shop for HEDIS quality and Stars management
Cotiviti’s Quality and Stars solutions support 44% of all MA contracts that received five stars in the 2026 Star Ratings. Read our fact sheet and learn how Star Intelligence enables health plans to:
- Get a clear view of progress with trending and benchmarking dashboards
- Leverage analytics that offer measure prediction, EOY predictions, trends, and opportunities for growth
- Get reliable insights through predictive cut points built into advanced analytics
HEDIS® is a registered trademark of the National Committee for Quality Assurance (NCQA).
CAHPS® is a registered trademark of the Agency for Healthcare Research and Quality (AHRQ).
