The evolution of physical therapy
Jonathan Edwards | Jonathan Lieberman MD, MPT, CHCQM-PHYADV, CPC-A | Roland Self

Physical therapy has evolved into a vital part of modern healthcare. Focused on physical interventions, treatments aim to restore patients to functional independence through exercise, stretching, manual techniques, and modalities. Once used primarily after injuries or surgery, physical therapy is now recognized as a key tool in managing chronic conditions, improving mobility, and deferring the need for operative intervention.
With rising patient awareness and a shift toward preventative care, physical therapy services are seeing sustained growth. A recent report found that there are more than an estimated 300 million physical therapy visits annually in the United States. According to the American Physical Therapy Association, all 50 states plus the District of Columbia and the U.S. Virgin Islands provide patients with some form of direct access to physical therapist services without requiring a prescription from a physician, making it one of the most accessible courses of care.
As the population ages and chronic diseases become more widespread, demand is growing for care that is non-invasive, cost-effective, and focused on long-term wellness. Physical therapy meets these needs by helping patients stay active, avoid unnecessary procedures, and recover more effectively.
A recent report found that there are more than an estimated 300 million physical therapy visits annually in the United States.
There is also an increased interest in “prehab” physical therapy services, which are initiated before major spine or joint surgeries. This proactive approach has been shown to improve quality of life by decreasing pain and opioid dependence; increasing balance, strength, and range of motion; and prolonging the time until the patient requires corrective surgery, sometimes indefinitely. Importantly, physical therapy is often mandated as a prerequisite for payment approval for these corrective procedures.
In this edition of Payment Policy Insights, we highlight three key trends across physical therapy in outpatient and professional settings and discuss the implications for health plans.
Demand for non-invasive care is increasing for an aging population
Physical therapy is a specialized yet high-volume service category that accounts for 6% of ambulatory claim lines and is the largest spend driver among therapy disciplines (physical, occupational, speech), according to Cotiviti data. These non-invasive services account for up to 93% of overall therapy spend, depending on line of business, with the highest expenses found in Medicare (Figure 1). This pattern has held steady and aligns with broader industry trends, pointing to continued growth in this area. Several drivers are likely contributing to this: an aging population, an increased prevalence of chronic conditions, more patients opting for non-invasive treatments, and the push for early intervention to avoid costlier care later.
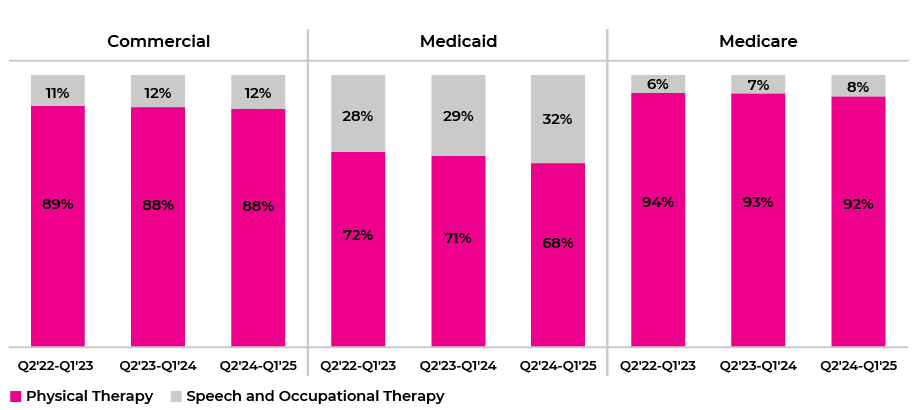
Figure 1: Distribution of spend by therapy discipline
Per Cotiviti data, overall physical therapy utilization (measured as claims per 1,000 members) has increased by a compound annual growth rate (CAGR) of 5% over the last three years, with the Medicare line of business alone growing as high as 9% (Figure 2).
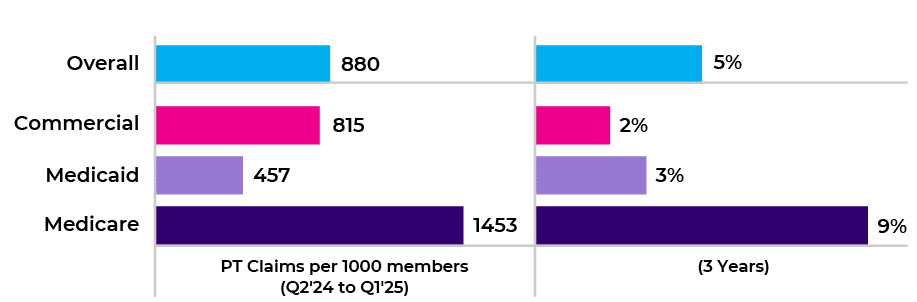
Figure 2: Physical therapy claim utilization and annualized growth by line of
business over three years
Excluding inpatient claims, physical therapy spend is mostly composed of professional claims, driving almost 62–80% of spend share (Figure 3).
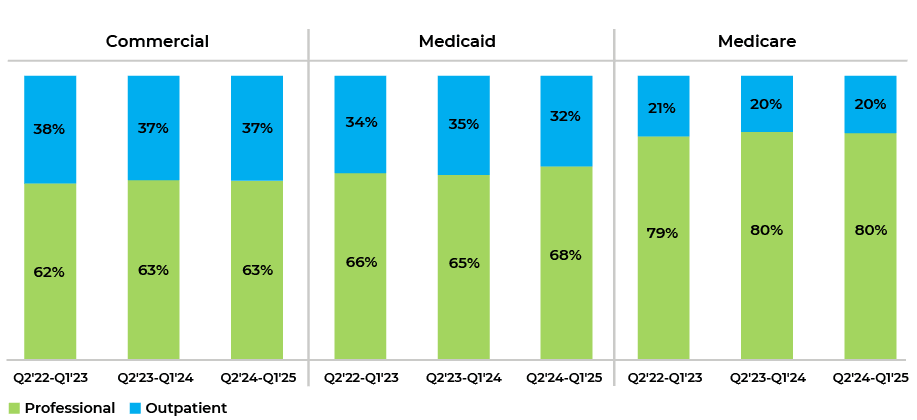
Figure 3: Physical therapy spend share by claim type across lines of business
For professional claims, physical therapy services are provided directly by a qualified provider such as a physical therapist or a physical therapy assistant under a physical therapist’s supervision. The professional spend is highest for Medicare (80%), likely reflecting the older population's need for more provider-led, in-person care in professional settings.
This contrasts with the outpatient claim type, where services are provided by facilities such as hospitals or comprehensive outpatient rehabilitation facilities (CORFs). Outpatient facilities offer a multitude of therapeutic services including physical, occupational, and speech therapies in addition to cognitive and cardiac rehabilitation services, all under one roof.
Musculoskeletal disorders are a key driver of physical therapy spend
Cotiviti data demonstrates that more than half of the ambulatory physical therapy spend is from therapeutic exercises and activities, which correlates with an increased focus on musculoskeletal disorders.
Just two out of more than 45 physical therapy procedure codes contribute to more than half of all physical therapy spend (Figure 4). Therapeutic activities focus on functional activities known as activities of daily living (ADLs), whereas therapeutic exercises directly strengthen targeted muscles and increase recruitment of motor neuron units involved in those functional activities.
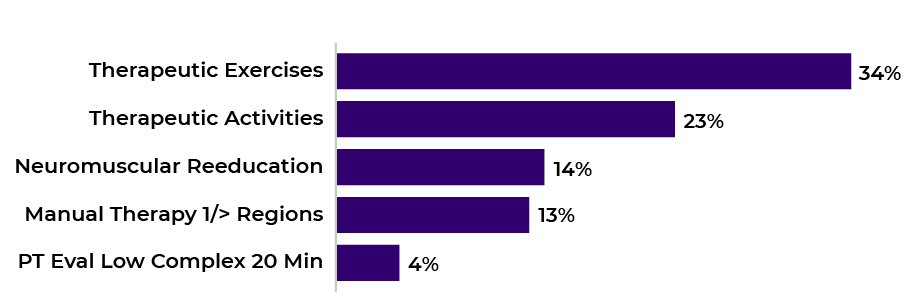
Figure 4: Top 5 Procedures by spend contribution in physical therapy services
According to Grand View Research, the orthopedic therapy segment accounted for nearly 59% of physical therapy provider revenue in 2024, driven by the rising prevalence of musculoskeletal disorders such as arthritis and a growing emphasis on nonsurgical injury rehabilitation.
This aligns well with Cotiviti’s data showing that the top five diagnosis groups—musculoskeletal disorders, back pain, neck pain, osteoarthritis, and joint derangement—account for up to 71% of professional physical therapy spending, with one-third from musculoskeletal disorders alone (Figure 5). The diagnosis distribution demonstrates a lower proportion of musculoskeletal disorders when moving from professional to outpatient claims, likely reflecting the relatively higher proportion of neurological disorders such as stroke, traumatic brain injury, spinal cord injury, and Parkinson’s disease predominantly treated at CORFs.
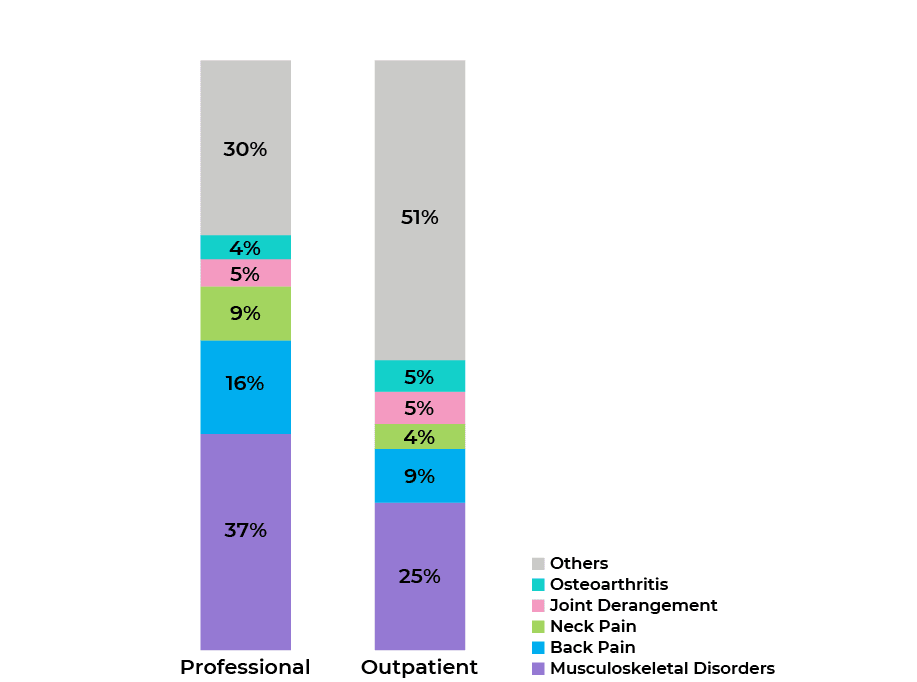
Figure 5: Physical therapy spend distribution by diagnosis groups*
Frequency and complexity of physical therapy services creates payment integrity opportunities for payers
Considering the increasing popularity of physical therapy being used as treatment for a variety of reasons, plans should pay close attention to billing errors and payment integrity opportunities. In fact, data from Cotiviti’s Payment Policy Management and Coding Validation payment integrity solutions shows that editing rates on physical therapy services are at least 50% higher than other medical services and procedures. Further, claim editing rates for physical therapy are higher than other therapy disciplines, highlighting the importance of applying a comprehensive policy set to these claims (Figure 6). Cotiviti data also reveals that the billing error rate for the latest year (Q2 2024–Q1 2025) for physical therapy services is nearly three times higher in professional settings compared to outpatient settings. This could be attributed to the previously mentioned increase in provider-led care within the professional setting.
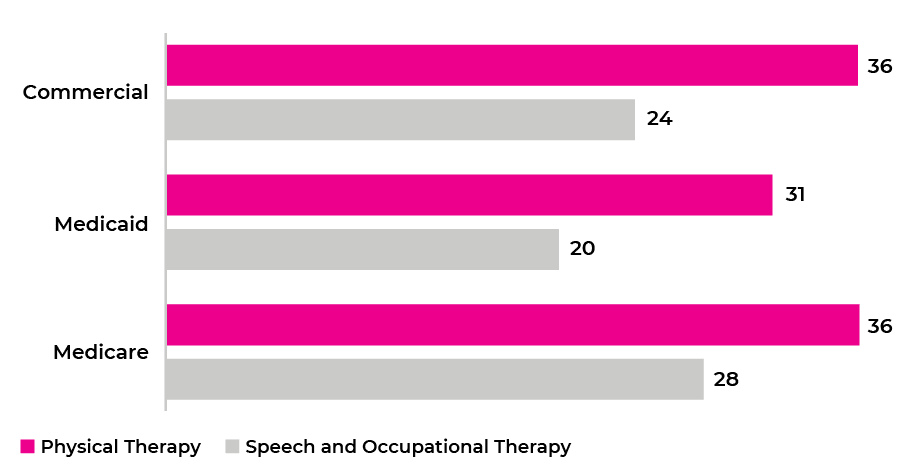
Figure 6: Edit per 1000 lines of physical therapy CPT codes vs other therapy services across lines of business
Cotiviti data shows that the Multiple Procedure Reduction for Therapy Services Policy in the Payment Policy Management solution contributes to over 50% of claim editing savings on physical therapy claims (Figure 7). Cotiviti’s Multiple Procedure Reduction policy applies a percent reduction solely to the practice expense component of additional same-day therapy services; it does not affect the work or malpractice components.
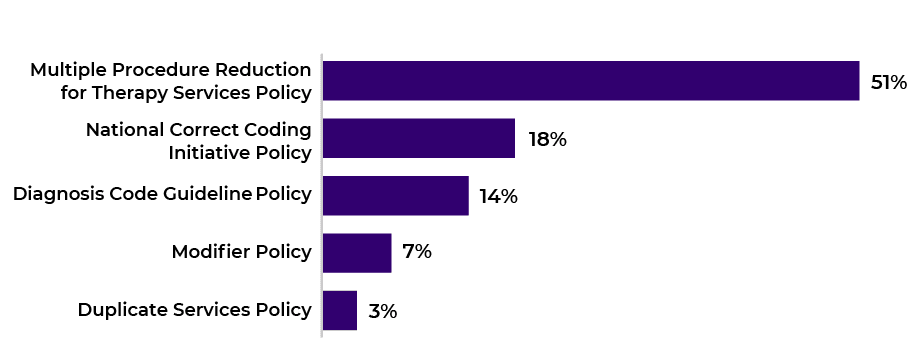
Figure 7: Top 5 Medical policies by savings on physical therapy claims
This Multiple Procedure Reduction policy does not generate substantial savings for Medicaid clients, perhaps due to many states not having published guidelines (i.e. being “silent”) on this topic. Instead, the Diagnosis Code Guidelines policy drives more than half of savings on therapy claims for Medicaid clients. This policy addresses coding to the highest level of accuracy and specificity by preventing certain ICD code categories such as external causes, manifestations, sequelae, and secondary-only diagnosis codes from being reported as the principal, first-listed, or only diagnosis. The Diagnosis Code Guidelines policy also addresses the ICD10 manual’s “Excludes 1” notes, which are used to indicate two conditions which cannot occur simultaneously and should not be coded together, such as contracture of joint (M24.5) and contracture of muscle without contracture of joint (M62.4-).
Cotiviti data shows that health plans with prepay modifier review programs via our Coding Validation solution capture up to 75% more payment integrity savings than plans only deploying automated code editing (Figure 8), depending on line of business. Most of these incremental savings are driven by conducting expert reviews of claims billed with modifiers that override traditional National Correct Coding Initiative (NCCI) edits, which accounts for an incremental 0.3-0.5% savings across lines of business.
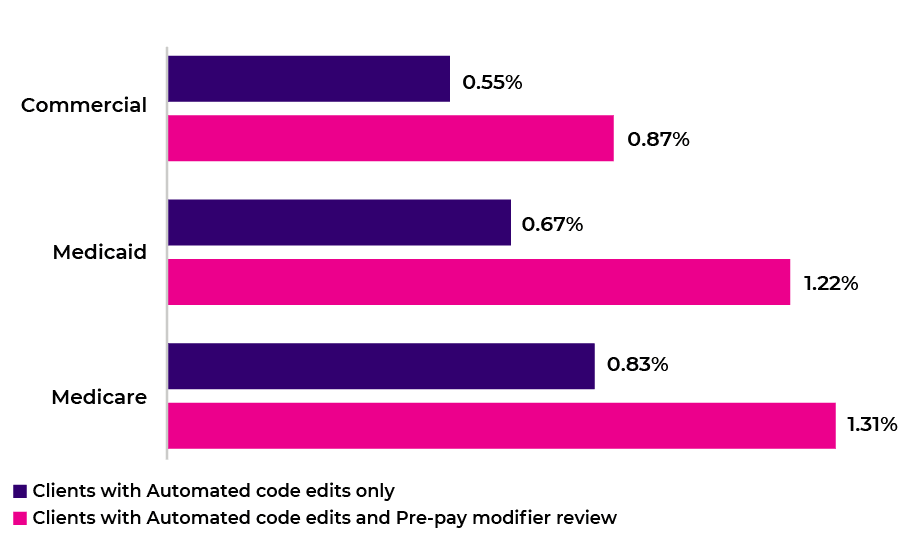
Figure 8: Comparison of savings rate on physical therapy for payers with and without prepay modifier review across lines of business (outliers treated)
Within Coding Validation for therapy services, much of the savings are due to National Correct Coding Initiative (NCCI) policies, emphasizing how correct coding remains the cornerstone for achieving optimal savings. Coding Validation can be used to flag a physical therapy claim for review to ensure appropriate use of bypass modifiers for certain therapy code combinations.
A common pattern observed in Coding Validation is the use of Modifier 59, which is intended to indicate that two services performed on the same day are separate and distinct. For example, if a physical therapist first performs manual therapy (97140) and then in a separately identifiable 15-minute increment later in the session performs therapeutic activities (97530), Modifier 59 usage may be appropriate.
On the contrary, there are situations where usage of Modifier 59 is not appropriate. For example, a physical therapist might submit Modifier 59 if they perform manual therapy (97140) on the lumbar spine followed by therapeutic exercise (97110) on a different region of the body such as the upper extremity. NCCI edits applied through Coding Validation would identify these services as Column 1/Column 2 pairs billed with Modifier 59. Upon Coding Validation nurse review, if it is determined that separate sessions, anatomical sites, or distinct clinical purposes were not supported, the modifier would be deemed inappropriate as the services should be bundled.
The value of physical therapy
Cotiviti insights demonstrate that physical therapy utilization is growing steadily, particularly among Medicare beneficiaries. Most spending concentrates on a few key procedures and diagnoses, reflecting the sector’s focus on musculoskeletal disorders and functional recovery. Strategic policy enforcement and prepay claim and modifier review are vital for payers seeking to manage costs and ensure payment integrity in this expanding area of healthcare.
If you would like to discuss your current physical therapy policy set within Payment Policy Management or want to learn more about modifier reviews through our Coding Validation solution, reach out to your Cotiviti representative or email us at answers@cotiviti.com.
*Percentages on chart may not total 100% due to rounding.
Physical therapy policies are just a small piece of Cotiviti's vast Payment Policy Management claim editing library.
Visit our Policy on a Page collection to read more about some of our other top policies.
About the authors
|
|
Jonathan Edwards Jon leads a talented team of analytic professionals that deliver actionable insights powering Cotiviti’s most important growth opportunities. With more than 15 years of healthcare analytics and consulting experience, Jon harnesses the power of data to develop leading-class analytic products and services that inform decision-making, accelerate growth, and differentiate Cotiviti’s value proposition. |
 |
Jonathan Lieberman MD, MPT, CHCQM-PHYADV, CPC-A Jonathan Lieberman is a Client Medical Director for Cotiviti, with over a decade of experience representing hospitals in Administrative Law Judge (ALJ) hearings for Medicare and performing peer-to-peer (P2P) reviews. He was a physical therapist prior to attending medical school, followed by completing his postgraduate training in general surgery and diagnostic and interventional radiology. |
 |
Roland Self Roland collaborates with a team of analytics professionals who deliver actionable insights to drive growth opportunities for Cotiviti clients. Following two decades in various client engagement roles serving payer clients, Roland leverages his healthcare industry and payment integrity expertise to develop analytical tools and services that support Cotiviti’s client teams to best serve our clients. This includes identification of best fit incremental growth opportunities associated benchmark analytics. |