Claim modifiers: Key trends and the value of prepay review
Jon Edwards | Brad Terry, MD, MBA, CHCQM, CPC | Lyndsay Majewski, MBA, RN, CPC

Modifiers provide crucial information for communicating the level of care for each member. According to Cotiviti data, claims with modifiers contribute to up to 47% of professional and outpatient medical spend and are an important component of healthcare billing and coding. But while modifiers provide details that might not be apparent otherwise, their complexity can lead to improper billing and payment integrity errors for payers. In fact, Cotiviti data shows that payer clients are capturing up to three times as many edits on lines billed with modifiers compared to lines billed without, emphasizing the need of prepay modifier review programs.
Prepay modifier review programs provide a substantial layer of protection against inappropriate billing for coding modifiers. These programs can mitigate some of the most common risks related to incorrect modifier usage, including financial loss, operational burden, compliance and legal risks, and others.
In this edition of Payment Policy Insights, we describe the purpose of claim modifiers, highlight important trends around modifier usage, and review how payers can help ensure modifiers are used appropriately.
The purpose of claim modifiers
There are two main types of claim modifiers: payment-impacting modifiers and informational modifiers.
Payment-impacting modifiers typically have a direct impact on the amount of payment received for a specific service or procedure. These can modify or reduce payment, such as when an entire product is not utilized as required with drugs and biologicals (D&B), or in the event that a surgery is either incomplete or stopped before occurring, in which case the reimbursement decreases and modifiers indicate that the entire procedure was not completed. Payment-impacting modifiers also include technical and professional modifiers, which indicate which portion of a service was performed. For example, when an X-ray is performed in an outpatient hospital, the physician, such as a radiologist, should only bill for the professional component and not the entire service since the facility will also bill for the X-ray and would result in overpayment to the physician.
Informational modifiers provide additional details about a service or procedure, but do not impact the pricing or reimbursement. They help to communicate specific details about the encounter, such as the reason for the procedure, the location of the service, or any other relevant information that may affect the medical coding process. These modifiers are essential for accurate documentation and communication between healthcare providers and payers.
The dangers of inaccurate claim modifiers
Improper use of either type of modifier can present significant risks for both the member and the health plan. These risks can include, but are not limited to:
- Financial loss. Overpayments could be in the form of direct loss with duplicative payments for the same service, or indirect loss when a health plan fails to capture important elements that are used for risk stratification of members, or to capture quality-related elements for members.
- Operational burden. Identifying, managing, and preventing overpayments requires resources and can lead to increased operational costs.
- Compliance and legal risks. Inaccurate payments (either over or under) can lead to compliance issues, as payers are expected to adhere to coding guidelines and payer policies, and may also be indicators of waste or abuse.
- Provider and member relations. Inaccurate payments can strain relationships with providers, especially if recovery efforts are not handled sensitively. If overpayments or underpayments are frequent or significant, they can damage the reputation of the payer, leading to a loss of trust among members and providers.
With these in mind, there are several trends around modifiers observed in recent Cotiviti data.
Modifiers drive a substantial amount of medical spend
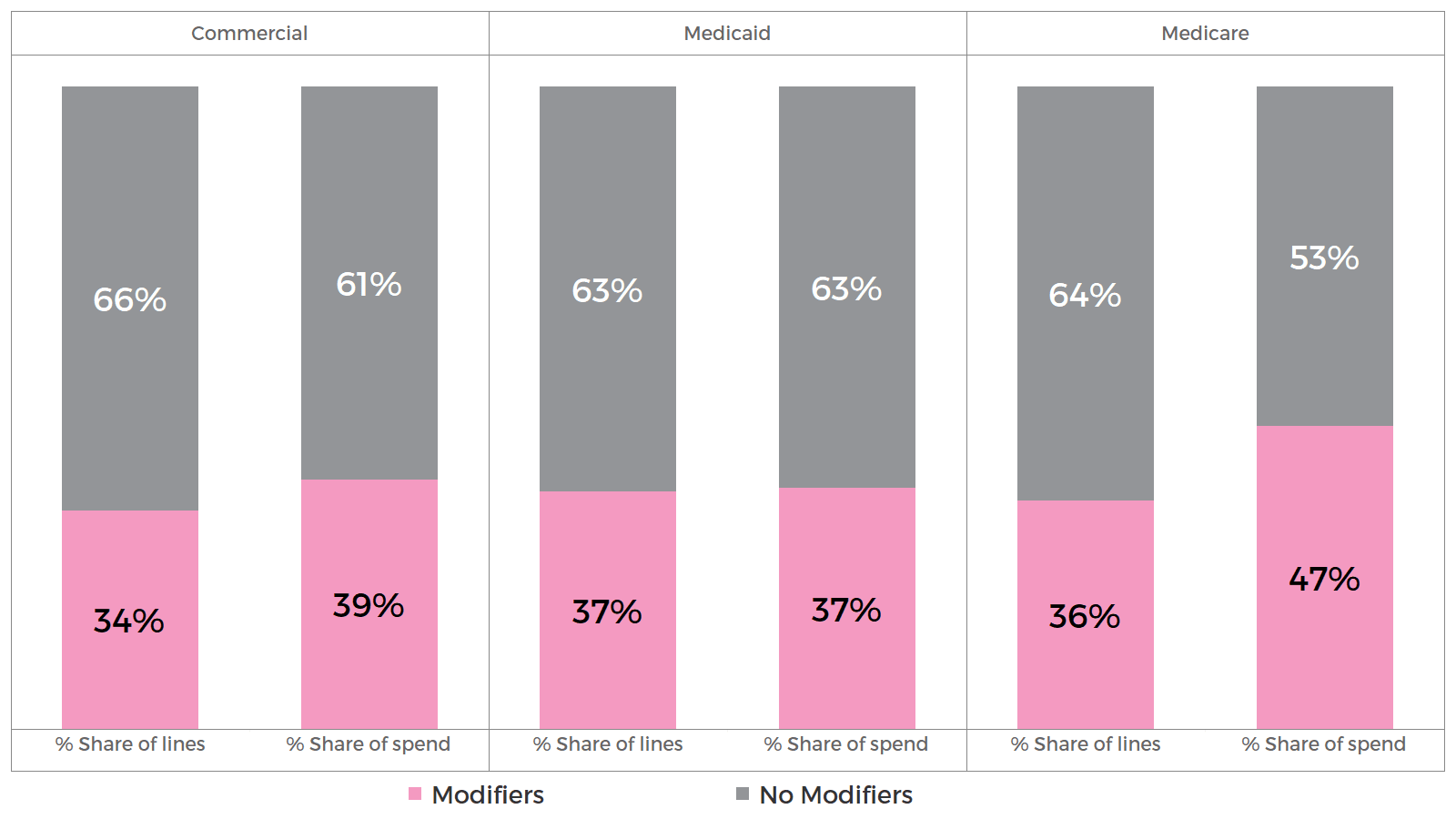
Up to 37% of medical claim lines are billed with modifiers, accounting for up to 47% of medical spend, depending on the line of business (Figure 1). This disproportionate impact on spend is driven by higher unit costs for claim lines billed with modifiers, reflecting that these claims often feature complex services or procedures.
Figure 1. Distribution of claim lines and spend by line of business.
Modifiers are more commonly reported on professional claim lines (approximately 40% of lines) compared to only 24% of outpatient claim lines, as most modifiers are specific only to professional claims. Outpatient claims use revenue codes and ambulatory payment classifications (APC) where only a limited number of modifiers are applicable. Given the higher use of modifiers on professional claims, it’s not surprising that more than 50% of modifier claim spend occurs in the office and home settings.
Modifiers are also used more within office and home settings in Medicaid and Medicare, contributing to more than half the spend billed with modifiers across these lines of business.
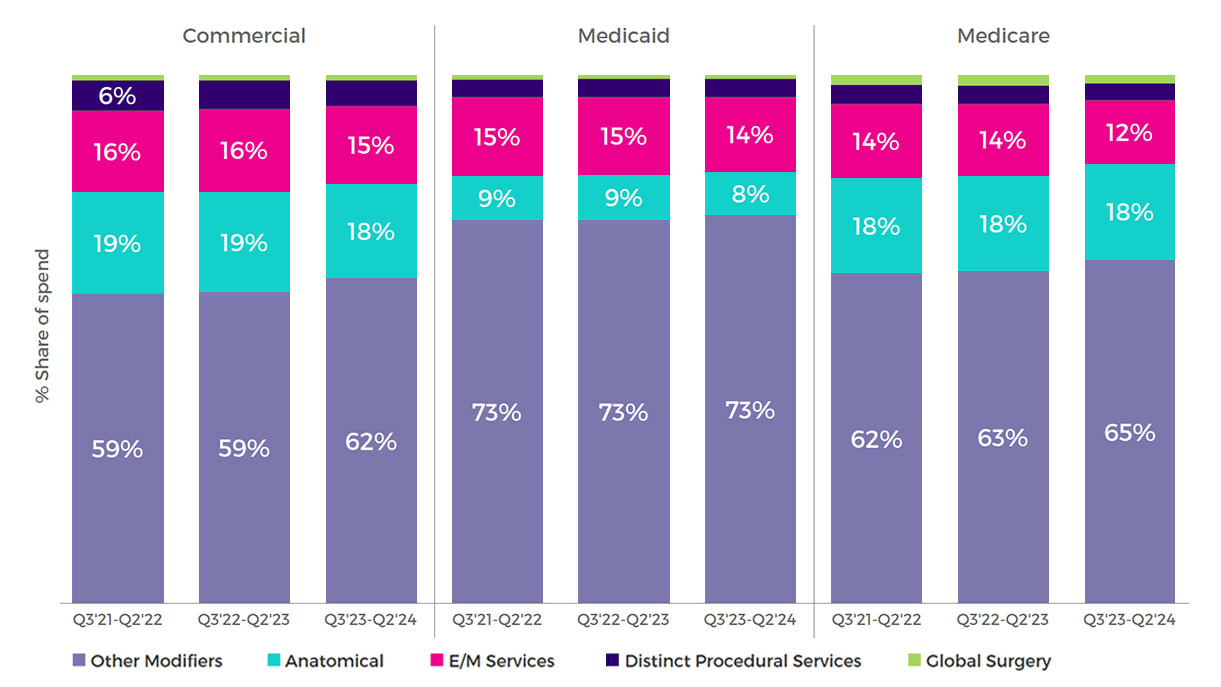
Evaluation and management (E/M) services, surgeries, medical drugs, and therapy services are the most common procedures billed with modifiers, and account for more than 65% of modifier spend (Figure 2). The rapid development of medical drugs (also known as biologics or specialty drugs) used to treat complex conditions has also contributed to an increase in modifier spend in recent years. Many drugs require weight-based dosing or dosing that does not utilize a full packaging size. Therefore, modifiers indicate whether the full or part of the drug package was used, determining how much a member is billed.
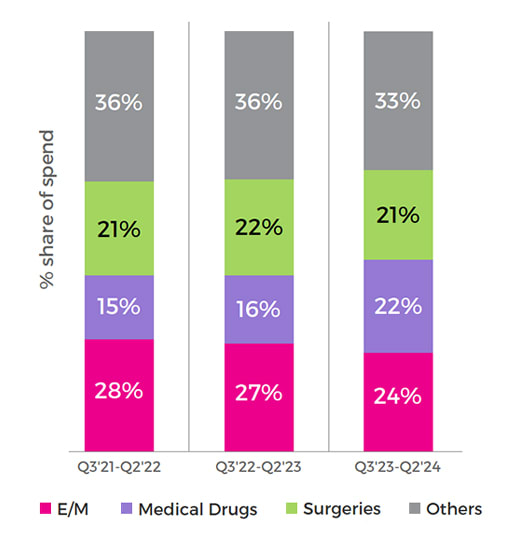 Figure 2. Distribution of modifier spend by service category.
Figure 2. Distribution of modifier spend by service category.
Modifiers address a broad range of clinical/coding concepts
There are hundreds of modifiers used in healthcare billing today, with 59 new modifiers introduced in the last five years. Modifiers are typically grouped into five categories:
- Anatomical procedures. These modifiers specify the location of procedures performed, with specificity that can range from which side to even a specific vessel in the heart. This helps ensure accuracy in both the short term and the long term for current and future procedures.
- E/M services. These types of modifiers are most commonly seen as modifier 25, which is used to indicate that a separate E/M service was performed on the same day as another procedure or service.
- Distinct procedural services. Procedures separate and distinct from other procedures reported on the same day by the same provider are reported with Modifiers 59, XE, XP, XS, and XU. These modifiers are often used for surgeries, medical drugs, and diagnostic procedures.
- Global surgery. Global surgery modifiers help clarify procedures or E/M services reported in the postoperative period of another procedure.
- Other modifiers. Many are used for medical drugs, reimbursement adjustment telemedicine, therapy, anesthesia, or durable medical equipment (DME).
Anatomical procedures, E/M services, and distinct procedural services modifiers contribute up to 38% of all modifier spend depending on line of business (Figure 3), with increasing unit costs across all groups.
Figure 3. Distribution of modifier spend by modifier group.
Outside of the four specific modifier groups noted above, Cotiviti data finds that most other modifiers impact claims for medical drugs, telehealth, therapy, anesthesia, and DME, among others.
Prepay modifier review programs capture up to 50% more payment integrity savings
Prepay modifier review is a proactive process implemented by health plans to analyze and validate the accuracy of modifiers attached to claim lines before payment. The review involves advanced analytics, clinical algorithms, and manual review by expert nurse coders to assess whether the modifiers were used appropriately. This process prevents improper use of modifiers to override claim edits, ensures compliance with coding guidelines, and maintains the integrity of the billing process.
For example, a prepay modifier review solution could flag a scenario in which a significant and separate service was performed, but where neither the claim data nor the documentation met the criteria for use of the overriding modifier. This is just one example of challenging coding scenarios often found on complex claims for vulnerable populations such as Medicare and Medicaid. Other examples of coding scenarios where modifier use should be reviewed include:
- E/M: A knee injection is performed as part of a series. An E/M should only be reported if a significant and separate service was provided in addition to the work associated with the injection.
- Distinct procedures: A dermatologist performs multiple procedures during a single encounter. Modifiers are used to identify areas of the body where the procedures were performed. To be separately reimbursed, each procedure must be separate and distinct from the others.
- Global surgical package: A surgeon evaluates a patient for incisional pain 14 days after a procedure with a 90-day global period. During this global period, all associated care is included in the payment for the original procedure. Only under specific circumstances can additional services be reported during this period. To accurately report these qualifying scenarios, specific modifiers are used supported by coding guidelines to accurately report the services performed.
- DME: A manual wheelchair was rented for a member. CMS guidelines limit the rental of a wheelchair to 13 months. Modifiers are required to accurately and appropriately reimburse the DME supplier as the reimbursement changes over the period of the rental.
- Medical drugs: Modifiers are used for medical drugs to indicate the quantity of medication used and wasted. Using appropriate modifiers ensures accurate payment for the medication utilized instead of the entire package, if not indicated.
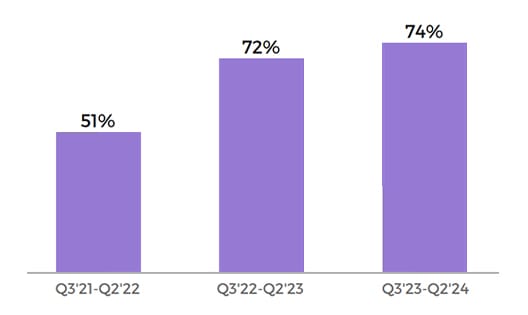
All of these applications are making prepay modifier review solutions more popular. Nearly 75% of Cotiviti’s prospective payment integrity clients have added prepay modifier review solutions, a trend that has risen from ~50% just a few years ago (Figure 4).
Figure 4. Adoption rate of Cotiviti prepay modifier solution (Cotiviti clients).
With a prepay modifier review program, health plans can catch unclear modifiers for better cost avoidance. Under NCCI guidelines, a modifier may be appended to a claim line to bypass editing only if the criteria for the modifier is met. Most claim editing platforms automatically override the edit and pay the line. However, Cotiviti has often observed that the NCCI criteria for the appropriate use of the overriding modifier are not met. Thorough review of appropriate modifier usage prevents incorrect payment.
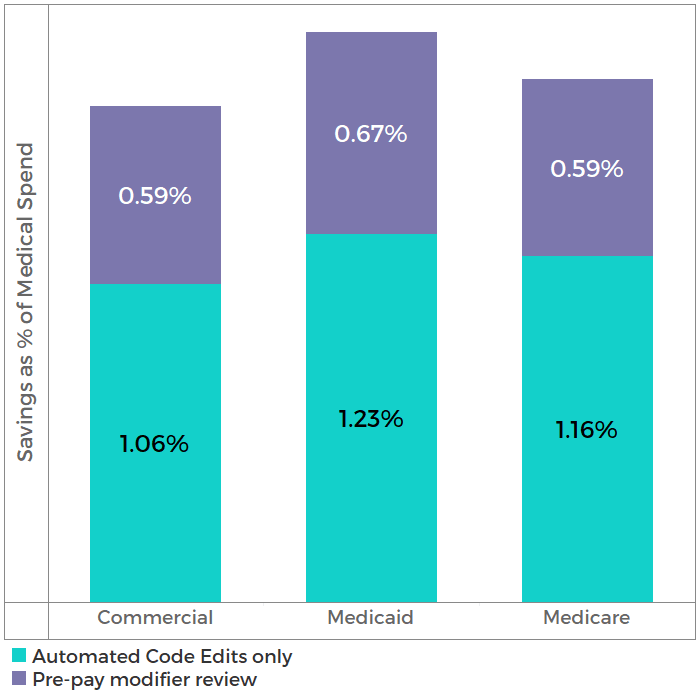
Cotiviti data shows that health plans with prepay modifier review programs capture up to 50% more payment integrity savings (as a percentage of professional and outpatient medical spend) on claims with modifiers than plans that do not have prepay modifier review programs (Figure 5).
Figure 5. Savings rate by line of business.
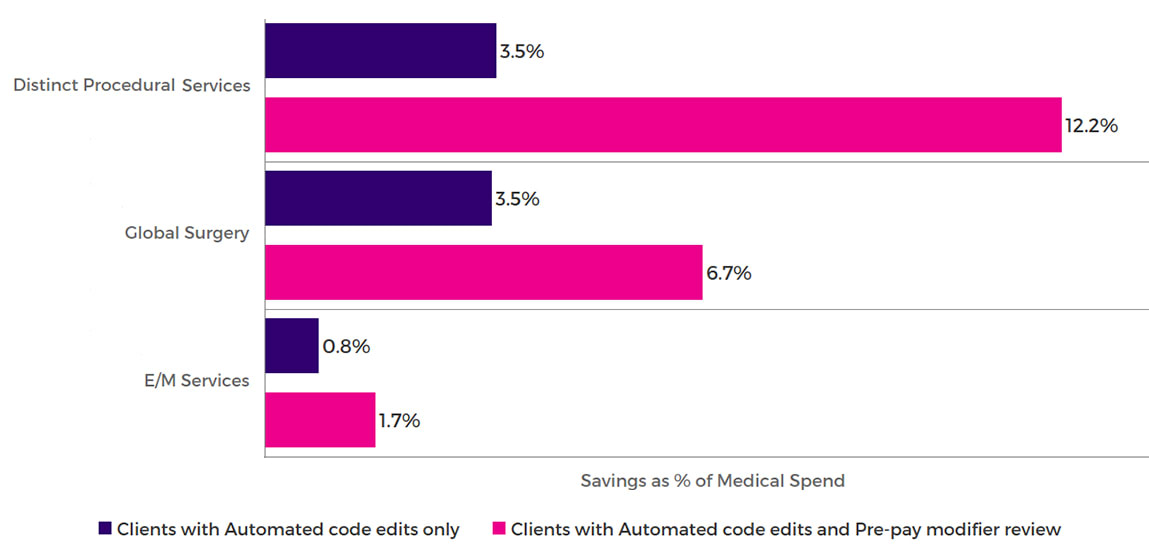
The incremental value of prepay modifier review can also be measured across specific modifier categories. Health plans with prepay modifier review solutions capture 2–4X more payment integrity savings on claims submitted with modifiers for distinct procedural services, global surgery, and E/M services (Figure 6).
Figure 6. Savings rate by modifier group.
Reduce inappropriate modifier use and improve payment integrity
Modifiers contribute to nearly half of professional and outpatient medical spend and provide information to help payers and providers deliver higher quality and more cost-effective care to healthcare consumers. They are also important reimbursement drivers, and with coding guidelines becoming increasingly complex and with new procedures and modifiers introduced every year, modifiers need to be used appropriately when billing claims.
This presents a significant opportunity for health plans to improve payment integrity and capture more medical cost savings on claims billed with modifiers. Health plans using a prepay modifier review solution as part of their payment integrity approach can realize incremental benefits and minimize losses due to incorrect billing.
Reduce inappropriate modifier use, improve payment integrity, and capture more medical cost savings with Cotiviti's Coding Validation solution. Even after primary and secondary claim editing, Coding Validation creates additional medical cost savings from identifying complex coding errors. Read the fact sheet or speak to your Cotiviti Client Engagement representative.
About the authors
|
|
Jonathan Edwards Jon leads a talented team of analytic professionals that deliver actionable insights powering Cotiviti’s most important growth opportunities. With more than 15 years of healthcare analytics and consulting experience, Jon harnesses the power of data to develop leading-class analytic products and services that inform decision-making, accelerate growth, and differentiate Cotiviti’s value proposition. |
 |
Brad Terry, M.D., MBA, CHCQM, CPC Dr. Terry is an experienced medical director who works with healthcare payers and hospitals to deliver high quality and cost-effective care. He blends clinical and analytical skills in a variety of medical and pharmaceutical areas from policy development, medical economics, and clinical programs. Dr. Terry has worked with Cotiviti assisting clients with prepayment solutions since 2021. |
 |
Lyndsay Majewski, MBA, RN, CPC Lyndsay is a healthcare payment integrity leader with over 25 years of healthcare experience. Her background includes registered nursing, healthcare payment integrity, data analysis, clinical documentation review, and appeals management. She specializes in Cotiviti’s Coding Validation solution and has been with Cotiviti for 11 years. |